As the orthopedic market shifts toward a focus on biocompatible and resorbable materials, magnesium is gaining momentum in trauma and sports medicine applications.
The use of magnesium is in response to the need for temporary — yet highly effective — implants. Hardware removal is one of the most common procedures performed worldwide and can be expensive, painful and present additional risks. On the other hand, leaving an orthopedic implant in the body can also pose potential risks for infection or other long-term failure.
A resorbable material removes those risks for indications where short-term fixation is needed, such as in fracture repair. However, current resorbable materials are typically made of polymers, which come with their own set of risks.
“If you look at the orthopedic space in total, generally we’re trying to do two things. We’re either removing a piece of diseased anatomy and replacing it, or we have anatomy that needs support to heal and to repair itself,” said Mark Hanes, Senior Technical Director at Genesis Innovation Group. “Current resorbables are typically polymers, which don’t have a good mechanical property profile for repairing bone. In some cases, you can use bio-ceramics, which again, don’t really have the right property profile to match bone.”
Polymer-based resorbables also tend to have a faster resorbable profile, meaning the potential is there to resorb before the bone can heal itself. An alternative material exists in magnesium, which is slower to resorb and allows for a more gradual transition back to a load-bearing bone.
“We see the potential for our magnesium alloys being used in orthopedic trauma fixation, sports medicine, extremities, craniomaxillofacial and dental reconstruction segments, as well as vascular and surgical applications,” said Adam Griebel, Senior Research and Development Engineer with Fort Wayne Metals, a materials supplier. “Our customers are very good at finding innovative ways to apply new technology.”
Benefits of Magnesium
Implants made of magnesium pose many benefits, including from a radiographic standpoint, a mechanical strength standpoint and an absorption standpoint.
“In terms of imaging, magnesium is absolutely ideal. Current polymer-based absorbable devices can be very challenging to diagnose or to image postoperatively and understand what’s actually happening with the device,” said Rob Ball, President and CEO of Magnesium Development Company, a Genesis Innovation Group portfolio company. “Throughout its absorption profile, it’s very visible on x-ray. And when you think about imaging related to sports medicine procedures, with magnesium, you can see where the anchors are, or where it is vs. where it started. But it also doesn’t interfere with surrounding tissues in an MRI circumstance.”


Magnesium Development Company (MDC) focuses on applying magnesium alloy to musculoskeletal implants, specifically foot and ankle and sports medicine indications. Their proprietary magnesium alloy technology and manufacturing method allow for high-strength, controlled absorption with a mechanical strength at least two times that of PEEK.
Magnesium occurs naturally in the human body, with about 60% of it stored within bones, according to the National Center for Biotechnology Information. So as the implant is absorbed postoperatively, it does not leave behind significant foreign material. In addition, academic studies have suggested that degrading magnesium implants may even enhance the healing of tissues, Griebel said.
Critical for bone health and development, magnesium also plays a key role in the absorption and regulation of calcium, and facilitates the transport of calcium across cells. Bone remodeling is also an important aspect of magnesium usage.
“There has also been a significant number of reports in literature related to inflammatory response to materials like polylactic acid and PLGLA, and while the device itself has been absorbed, it certainly has not left behind a natural anatomy as it existed prior,” Ball said, referring to commonly used polymer resorbables.
As device companies explore ways to provide safer, recovery-promoting solutions, they’re turning more and more to magnesium alloys and magnesium ceramics.
“Magnesium is one of the few resorbable metals that exists,” Hanes said. “So it is able to fill that niche of allowing the anatomy to heal and then just resorb.”
Leveraging Magnesium in Orthopedic Products
Bone Solutions, a company specializing in magnesium-based biologics, started using magnesium several years ago to create their OsteoCrete FDA-cleared bone void filler. Their proprietary formula uses magnesium oxide, which is a natural compound mixed with various sulfates to create strong bone regenerative capabilities.
“This enables really good osteosignaling pathways and the magnesium phosphate crystallization, which also creates a mechanical bonding product,” said Drew Diaz, President and CEO of Bone Solutions. “It binds with the same type of properties as PMA for bone-to-bone or metal-to-bone. The importance of magnesium is that it really helps with the signaling pathways. It also provides the osteoblast with the capability of laying down the collagen fibers (the fibers for bone remodeling).”


Bone Solutions started using magnesium several years ago to create OsteoCrete, an FDA-cleared bone void filler. Their proprietary formula uses magnesium oxide, which is a natural compound mixed with various sulfates to create strong bone regenerative capabilities.
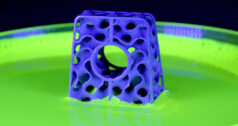
Recently, the company has sought to blend their magnesium technology in various ways to create pins, screws, anchors and even small plates. They are currently in vivo testing these products, with the aim to have an FDA-cleared, resorbable magnesium phosphate ceramic implant by 2023. These magnesium phosphate ceramic implants can be 3D-printed or injection molded.
“As our implant gets resorbed, it’s a creeping substitution that’s taking place,” Diaz said. “Our volume is maintained, so the structural integrity is maintained, and then it’s replaced gradually by remodeled bone. What we’ve seen with magnesium phosphates is that because of the magnesium, and because it’s so important to bone regeneration and proper bone healing, we have not had an incident where the implant was resorbed and not replaced with remodeled bone. Not one to date.”
Magnesium Development Company (MDC) focuses on applying magnesium alloy to musculoskeletal implants, specifically foot and ankle and sports medicine indications. Their proprietary magnesium alloy technology and manufacturing method allow for high-strength, controlled absorption with a mechanical strength at least two times that of PEEK. They are developing devices initially for interference screws used in ACL repair, along with other applications in knee and shoulder, sports medicine and foot and ankle repair.
“We’re providing exactly the same form factor that the marketplace is accustomed to today, but providing it in a form that provides absorption over an appropriate period of time,” Ball said.
Likewise, Finnish orthopedic device company Bioretec’s RemeOs Screw is a bioabsorbable metal implant currently undergoing clinical trials. The screws are based only on magnesium, calcium and zinc, which all occur naturally in the body. Depending on the size, the RemeOs screws absorb fully within two to three years after implantation. FDA recently granted the RemeOs Screw a Breakthrough Device Designation.
RemeOs screws were recently tested in a clinical trial to repair medial malleolar fractures. According to Biorec, as early as 12 weeks post-surgery, all the fractured bones were completely healed. No adverse events or complications have been observed in any of the patients tested during the one-year follow-up.
Regulatory Considerations
It’s no secret in the medical industry that introducing new products — and in particular, new materials — is difficult. The team at Fort Wayne Metals has advice on the material side of the process.
“A new alloy designed to dissolve into the body requires an order of magnitude more study than a new non-degrading material,” Griebel said. “Understanding the degradation rate of the device is one of the biggest challenges, as it will be impacted by alloy composition, material condition, implant size and location, and if any coatings have been used. There are more minor considerations as well; for example, magnesium is relatively reactive even to moisture in the air, and users need to use great care in proper handling and storage so as not to unintentionally alter the material surface.”
On the device side, the challenges that come into play revolve around the interactions with FDA and getting the agency comfortable with both the technology and the process of proving the devices are safe and effective.


Bioretec’s RemeOs Screw is a bioabsorbable metal implant currently undergoing clinical trials. The screws are based only on magnesium, calcium and zinc. Depending on the size, the RemeOs screws absorb fully within two to three years after implantation.
Magnesium Development Company was granted a Breakthrough Designation for their material technology. They have been working with FDA since 2014 on various animal studies to identify and mitigate risks as they relate to the application of the device.
“It’s both the opportunity and the challenge,” Ball said. “While it does represent a challenge in terms of the speed to which we can arrive in the marketplace, it represents a great opportunity because it can put us in an exclusive position having gone through this relatively challenging process with the FDA.”
The orthopedic device companies understand the rigor and detail necessary to jump regulatory hurdles. Gathering the data is a vital part of ensuring a product’s safety and effectiveness and proving its outcomes.
“One of our biggest challenges was acquiring that data,” Diaz said. “We have it now. The other challenge for a small company is distribution.”
Bone Solutions’ OsteoCrete was a predicate that had already been FDA-cleared. As the company expands their portfolio of products, they’re using the formulation of the already-proven OsteoCrete.
The use of magnesium in resorbable or temporary implants is on an upward trajectory. The companies we interviewed anticipate a continued acceleration over the next decade. Diaz expects many of the calcium phosphate products currently in use to be replaced with magnesium in five to 10 years. It’s already happening now, he said.
Ball anticipates widespread adoption of magnesium in foot and ankle reconstruction. “The concept of having a device that does not need to be removed is obviously attractive for payers, providers and patients — all three stakeholders win in that scenario,” he said.
Likewise, material suppliers are noting the trend.
“Within five years, we expect to see a handful of orthopedic magnesium devices on the market in the U.S.,” Griebel said. “In 10 years, we believe the use of magnesium implants will have become common practice for a wide range of indications.”
HT
Heather Tunstall is a BONEZONE Contributor.