Titanium, stainless steel and cobalt chrome implants have been mainstays in joint replacement surgery for decades, but OEMs have turned to alternative materials to improve outcomes as patients continue to experience dissatisfaction with their results and undergo revision surgeries to fix prosthesis failures.
Orthopedic companies want to address the concerns of roughly one in five patients who don’t like how their new knees feel and function.
“Manufacturers are now designing implants with medical congruent bearing articulations that mimic the normal knee,” said Jim Lancaster, President of Global Reconstructive Business at Zimmer Biomet.
The latest joint replacement implants are designed to provide added durability, stability, low-friction bearing, improved wear resistance, simpler fixation and greater range of motion.
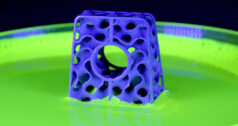
Manufacturers have recently introduced cobalt-free, cementless and advanced porous titanium systems to improve bone fixation and long-term outcomes. Additionally, advances such as additive manufacturing (AM) have led to the creation of personalized and patient-specific implants.
“Current trends in implant designs involve a more personalized approach to surgical care as manufacturers attempt to match the natural kinematics of individual patient’s knees,” said David Conley, Senior Director of Hip and Knee Marketing and Product
Development at Medacta USA. “Newer materials and manufacturing techniques allow manufacturers to fine-tune implant porosity to mimic natural bone, which increases bony ingrowth and prevents implant subsidence over time.”
Alternatives to Cobalt and Cement
The orthopedic industry is trending away from the use of cobalt chrome implants and focusing on new materials and ceramic coatings to reduce or eliminate cobalt ion release into the body.
Concerns about the use of cobalt chrome stem from wear associated with metal-on-metal implants that causes small amounts of metal to enter the patient’s bloodstream and increases the risk of cobalt toxicity, which can affect multiple organs. Further, the material faces scrutiny by regulatory bodies like the European Commission.
“Implant companies are replacing cobalt chrome implants with innovative materials (such as TJO’s Aurum Technology) or titanium niobium nitride coating technology (Medacta’s SensiTin coating, for example) to eliminate or reduce cobalt ion release,” Conley said.
Cemented implants present several risks, including thermal damage, monomer toxicity and cement breakdown that can cause loosening and debonding of the implant. Stress on the joint causes the cement used to fix implants in place to break down over time, releasing fragments of cement into the body.
Cementless total knee arthroplasty (TKA) addresses these issues. The technique isn’t new and various cementless implant designs have demonstrated excellent long-term survivorship, but its use is not yet widespread.
That trend is changing. Recent data from the American Joint Replacement Registry showed cementless TKA utilization increased from roughly 4.5% in 2017 to just over 14% in 2020.
“Cementless joint replacement helps reduce the untoward effects of cement in the body and reduces surgical times, as surgeons don’t need to wait for the cement to cure,” Conley said. “Through the use of innovative 3D metal printing techniques, manufacturers are able to produce cementless implants with bone-friendly porosity, while still maintaining strength and stability in the constructs.”
Tibial loosening continues to be among the most common causes of total knee replacement revision when cemented implants are used, according to Lancaster. Zimmer Biomet’s OsseoTi Technology leverages 3D printing to produce a cementless, porous metal implant that reduces this risk by mimicking the architecture of cancellous bone.
“Bone cement debonding and breakdown can contribute to tibial loosening, and pieces of broken cement can cause bearing wear,” Lancaster said. “These risks are minimized by forgoing cement and using an implant that provides biological fixation.”
Improved Longevity
OEMs are using antioxidant polyethylene to reduce instances of stress shielding around metal implants and wear resistance of bearing materials that cause osteolysis.
“Highly crosslinked antioxidant polyethylene limits the amount of polyethylene wear debris, which can cause osteolysis in the surrounding bone and lead to early implant failure,” Conley said. “Metal 3D printing technology produces implants that more closely mimic supporting bone and help increase the speed and ability of the bone to interdigitate with the implant surface.”
Lancaster said that antioxidant polyethylene allows implants to maintain high mechanical strength, wear resistance and oxidative stability, which are important for the long-term integrity of the material. For example, Zimmer Biomet’s Vivacit-E Vitamin E-based Highly Crosslinked Polyethylene with antioxidant protection produces a high wear-resistant material that reduces the risk of osteolysis.
Other manufacturers have launched titanium-based implants or titanium surface coatings. Smith + Nephew recently introduced the JOURNEY II ROX Total Knee Solution, a reverse hybrid construct for total knee replacement that combines several technologies — including advanced porous titanium and the wear resistance of oxidized zirconium — to provide long-term tibia fixation of a cementless knee.
Searching for the Holy Grail
The development of medial congruent bearings and cementless total knee replacement will continue, according to Lancaster, who added, “Use of cementless implants and cobalt chrome alternatives for partial and revision knees will also increase.”
Orthopedic manufacturers’ efforts to eliminate cobalt in implants will continue over the next five years with 3D metal printing and non-toxic materials, such as ceramic and polyetheretherketone (PEEK), Conley said.
Demand for improved knee replacement outcomes drives innovation in implant materials as manufacturers look to increase the longevity, safety and performance of the devices. Advancements in 3D printing and robotic assistance also enable surgeons to place the hardware with increased accuracy and precision.
“Implants mimicking the knee’s natural kinematics will gain traction and surgical techniques will continue to evolve, driving knee replacements toward the ultimate holy grail of the ‘forgotten joint,’” Conley said.
HT
Heather Tunstall is a BONEZONE Contributor.