Stefan Kreuzer, M.D., is an orthopedic surgeon and the founder of INOV8 Orthopedics, a Houston-based practice that integrates technologies such as robotics to improve patient outcomes. Regarded as a savvy innovator in orthopedics, Dr. Kreuzer is credited for helping to develop minimally invasive and computer-assisted hip and knee replacement surgery and is frequently asked to demonstrate his surgical techniques for surgeons throughout the United States, Asia and Europe.
To gain insights into the complex and ever-evolving relationship between robotics and orthopedics, we interviewed Dr. Kreuzer just two days after the surgeon pioneer performed the world’s first procedure using the second-generation TSolution One® Total Knee Application for total knee replacement.
Congratulations on your recent surgical achievement. Can you explain the role that robotics played in the knee replacement procedure?
Dr. Kreuzer: That was the first case performed with the new platform of the autonomous robot developed by Think Surgical. I’ve been involved with Think Surgical on the development side as well as on the FDA clearance side. The robot has been upgraded on two fronts. The actual robot itself is much more robust, has more flexibility, and has improved some accuracies as well. The planning platform has also been significantly improved, and it gives me more options. It’s an open platform, so we have more choices for different implants. Also, the planning gives me more flexibility to place the implant exactly where I feel is best for that patient.
We’ve heard from some surgeons that the level of robotic sophistication in orthopedics compares unfavorably to other industries. How would you characterize the current capability of orthopedic robots?
Dr. Kreuzer: If you compare robotics in orthopedics to other industries, I think where we are somewhat in an infancy with robotics in orthopedics is in two areas. Number one, we have not done a good job of publishing accuracy data. If you look at all the different platforms currently on the market, they really do not publish accuracy. There are two different types of accuracies: dimensional accuracy and positional accuracy. Until you define those two degrees of accuracy, you can’t really say something is more or less accurate if you don’t publish the data. That’s one area that we’ve not done a good job. Second, one of the nice things about robotic surgery is that it’s a data-gathering machine. With Da Vinci surgery, they collect all the motions that you perform with your hands. They’ve used artificial intelligence to go back and see which motion correlates with urinary incontinence or some positive clinical outcome to train us to become better surgeons. The Da Vinci platform does that, and in general surgery, they do a lot of that AI-driven data-driven stuff that we really don’t do in robotics. Those are the two areas where we are really behind. A strong focus needs to be placed to confirm that robotics is actually clinically relevant in orthopedics.
What do you think the best argument is clinically for the extra cost of robotics in orthopedics?
Dr. Kreuzer: Currently, I can’t quote a well done paper profiling a randomized control trial that can say that a robot performs better. Everybody thinks robots are more accurate, and they probably are, but we have to prove that. I think where robots really do play a positive clinical role is by eliminating outliers. We are more consistent. For the community surgeon who does 20 knees a year, if he does them with a robot, he will probably hit the target more often than not. The surgeon who does 300 knees a year is probably just as good with conventional instruments as he is with a robot. But that’s where we still need those randomized controlled trials.
Those trials need to be done to prove the clinical relevance of the robot. Now, the other areas, economic relevance. There are two different categories to look at. First, is there an economic benefit for the end user, the hospital, and the surgeon? And second, is there a benefit to the device companies who sell the robots? From an economic standpoint, the hospital may have some benefits in increasing their surgical volume being a destination center so they can tout their robotic program as a center of excellence.
On the device company side, the economic benefit is decreased inventory and instrumentation because, with robotics, you need far fewer instruments, and instruments are expensive. Essentially, you could eliminate inventory in the field because with certain robotic platforms, if you plan a size five femur, like the one that we did on Tuesday, it’s going to be a size five femur, not a four or a six, but a five. The device companies have an enormous amount of inventory in the field that costs them a lot of money. With a robot platform, you can essentially eliminate inventory in the field.


Stefan Kreuzer, M.D., and his team at INOV8 Surgical were the first healthcare facility to utilize the second-generation TSolution One by THINK Surgical. Photo Credit: Brandi Peace, INOV8 Research
What elements or capabilities must a new robotic system possess to be considered truly “next-generation” to you?
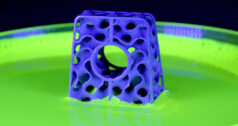
Dr. Kreuzer: There are a couple of areas that get me excited about the next generation of robotic platforms. It’s the autonomy, cutting features and the different cutting tools that cut different shapes. Most platforms currently on the market use an oscillating saw, but with an oscillating saw you can only make flat cuts. With an autonomous robot, you can program any cutting tool to cut any shape. So that really expands your potential indication.
For the next generation to be an autonomous robot, I prefer open platforms. An open platform robot gives the surgeon many more choices because every implant has a different kind of nuance, and what might be the right implant for Mr. Jones may not be the right implant for Mr. Miller. If you have an open platform, you have many more implants at your disposal to match the right size with the right patient. The merging of a custom implant with an autonomous robot is critical because an autonomous robot is going to be more accurate than the current robots on the market. A custom implant has less margin for error because it’s custom made to suit just one patient. So, if I make a custom suit for you and give it to my brother, it’s not going to fit well with my brother because he has different dimensions than you do. A custom implant will function better and more predictably if placed very accurately, and this can be achieved with an autonomous robot.
Where do you see the current adoption of robotics? What do you see as the primary obstacle to increased adoption and regular usage?
Dr. Kreuzer: I think the adoption will continue to increase, but I don’t think it will be quite as fast as some people say, and that’s going to be driven by the pressure of one surgeon getting more business than another. The biggest hurdle is cost. Robots are expensive, and they increase the per-case cost. And with the push of Medicare going to an outpatient setting where the reimbursement is less than $10,000, there’s going to be a huge price pressure on robotic platforms. They’ll have to figure out how to include that into the bundle for these lower-cost payers. In my opinion, what will drive the adoption even more will be if there are better proven clinical outcomes. Again, I can’t emphasize this enough, this can only be proven with randomized controlled trials where you perform surgeries on one patient with a robot and another patient without a robot. Then, you see who requires less physical therapy, has less pain, takes less opioids, who recovers faster, who goes back to work faster. If the patient with the robot has better-proven outcomes, then the ROI is there. Then, these platforms will almost be demanded.
PM
Patrick McGuire is a BONEZONE Contributor.