In February, Medtronic bought the rights to Nanovis’ nano surface technology that improves the biological fixation of orthopedic and spine implants. Medtronic intends to employ the bone-growth nanotechnology to develop PEEK interbody spine fusion devices.
The move provides a glimpse into how orthopedic companies view the future of device designs. Brian More, Nanovis CEO, pointed to a lack of innovation in terms of the materials used to produce spine implants — PEEK and titanium have been the mainstays — and said the market was primed for something new. Enter his company’s surface solution.
“Now, we’re starting to see that same dynamic emerge in other areas,” he said. “As markets mature and implants start to look the same, orthopedic companies will begin to explore innovative ways to make devices perform better.”
Expanding Applications
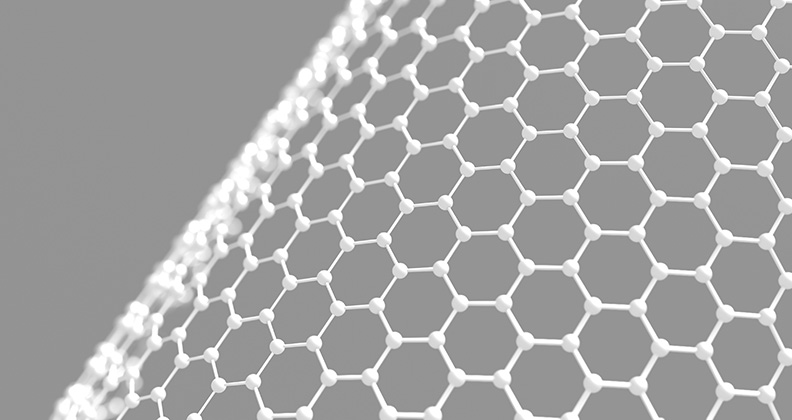
Nanovis’ nanoVIS Ti Surface Technology can be applied to pure titanium and titanium alloys to increase and accelerate biological fixation. “The implant surface is permanently restructured to create nano features, not just coated, to ensure a consistent biological response,” More said.
When proteins absorb onto the nano surface, the spacing between them sends a signal to the body to initiate bone cell proliferation. The nano-scale features also reduce bacterial attachment, improve inflammatory response and enhance vascularization.
Nanovis focuses on “four pillars of healing” by creating an optimal implant surface for cell attachment, promoting vascular growth, encouraging a healthy inflammatory response and reducing bacterial attachment. The company believes that implant surfaces can be engineered to achieve specific healing goals.
“We’ve identified that certain nano dimensions enhance osteointegration, while others improve soft tissue attachment,” More said. “We’re now focused on developing a portfolio of tunable surfaces to address various orthopedic needs.”
More noted that implant manufacturers approach his team with device designs that require optimal osseointegration and areas where soft tissue needs to exhibit strong attachment or no attachment at all.
“Nanostructures can be precisely engineered to address those needs — encouraging tissue attachment and osseointegration where desired or being hydrophobic to prevent tissue adhesion in specific areas,” More said.
Nanovis chose to initially apply its nano surface technology to a series of spinal interbody devices and pedicle screws. In the past two years, More and his team have focused on expanding the company’s portfolio to include a wide range of applications.
“We believe the next big opportunity is in foot and ankle, particularly with challenging procedures,” he said. “Many patients — whether due to conditions like diabetes, autoimmune disorders or medications that trigger autoimmune responses — tend to heal poorly. The challenge becomes even greater when dealing with the distal extremities, where decreased blood flow, conditions like neuropathy and other factors impact how well the body heals.”
More also believes nano surface technology can make a significant impact in trauma care, where infection is a key challenge and concern. His team has tested five different bacteria strains and observed a reduction in bacterial attachment, ranging from two-thirds to 1.5 logs due to the nanotechnology’s surface dimensions.
“The surface area needs to integrate and protect,” More said. “We’ve found that if you manage bacterial attachment effectively while also focusing on the other key design pillars — osteointegration, vascularization and immune system engagement — you naturally reduce the risk of infection.”
Industry’s increased interest in cementless knee implant fixation also presents a growth opportunity for nano surface technology.
“The porous surface structure of a cementless implant plays a big role in achieving strong terminal fixation, and with a nano surface on top, fixation becomes even faster,” he said. “With cementless knees, for which terminal fixation and fast fixation are critical, nanotechnology can make a substantial difference.”
Sharing the Load
Nitinol, a nickel-based titanium alloy, provides two main benefits in orthopedic implant design according to Scott Robertson, Vice President of Nitinol Technology at Resonetics.
First, the material has a much lower stiffness compared to titanium or stainless steel — closer to that of natural bone — so the risk of stress shielding is reduced.
“Because nitinol is more elastic and compliant, it transfers load more naturally to the bone, helping to preserve bone health,” Robertson said. “That’s a big benefit, but it’s not widely used yet in load-bearing applications.”
The second big benefit of nitinol involves applications that require a constant, sustained load — in surgical staples, for example.
“With most conventional materials — stainless steel, titanium and even PEEK — the staple provides an initial squeeze, but the compressive force drops off as the material relaxes,” Robertson said. “The staple behaves like a traditional spring. As it unloads, the force decreases.”
Nitinol behaves completely differently. As it deforms, it maintains a constant force over time, even as bones move or settle. “That’s a game-changer in applications where steady compression is critical for healing,” Robertson said.
Eric Veit, Vice President of Business Development at Resonetics, believes that nitinol is underutilized in orthopedics even though it provides real advantages that could benefit a wide range of applications. “Because of the material’s mechanical advantages, especially its combination of flexibility and durability, there are many more ways that it could be used,” he said.
For example, thin bone plates made from nitinol would provide strength and elasticity. They would conform better to bone and stay in position under dynamic loads. Nitinol suture anchors or other soft tissue fixation devices could provide constant tension over time. Nitinol spinal implants would be strong yet forgiving, and actively support healing.
There are clear benefits to using nitinol to produce orthopedic implants, but perceived barriers need to be addressed before the material’s adoption becomes more widespread.
One is manufacturability.
“Unlike titanium or stainless steel, nitinol doesn’t machine well with standard CNC processes,” Robertson said. “Engineers and machinists run into tool wear, high scrap rates, yield issues and a steep learning curve.”
The perception that nitinol is costly and difficult to work with has also stalled promising projects involving the material. A few companies, like Resonetics, have worked with nitinol for decades and understand the unique aspects of the material.
During heat treatment, for example, even a five-degree difference in temperature or a minute or two difference in duration can significantly alter nitinol’s mechanical properties.
“We’ve refined the processes, optimized the tooling, and proven that you can achieve yields and costs that are on par with traditional metals,” Veit said. “For product developers who are new to nitinol, working with the right manufacturing partner can be the difference between success and a really expensive learning experience.”
OEM customers approach Resonetics with as much information as they have about the proposed product, and the team assesses not only what’s written in the spec but also what’s not included — and should be.
“More often than not, the specifications we receive are under-defined — not because the customer lacks expertise, but because they’re unfamiliar with how nitinol behaves,” Veit said. “We can either help refine and improve their specification or build a part that not only meets the spec but also performs the way they need it to.”
Once more implant design teams understand the benefits of nitinol and begin incorporating it into their products, clinical evidence and real-world performance will be needed to show that the material offers a meaningful benefit over other materials.
“The adoption curve is still early, but it’s shifting,” Veit said. “The more engineers and surgeons understand how nitinol behaves — and how it’s fundamentally different from conventional alloys — the more they’ll start to see its potential.”
DC
Dan Cook is a Senior Editor at ORTHOWORLD. He develops content focused on important industry trends, top thought leaders and innovative technologies.




