Last January, 3Spine announced that it had achieved enrollment for the U.S. clinical trial of the MOTUS lumbar total joint replacement system. The trial was launched after the device secured FDA Breakthrough Device Designation and Investigational Device Exemption in 2020.
The achievement had been two decades in the making.
During the early parts of their careers, MOTUS Co-inventors Scott Hodges, D.O., and Craig Humphreys, M.D., realized that lumbar fusion patients were not achieving the outcomes they expected, even when their x-rays appeared satisfactory. These disappointing results led him to conduct research beginning in 2004 that focused on Kambin’s Triangle and load methodologies. That ultimately led to a pilot study involving nearly 100 patients in 2017, the results of which were instrumental in 3Spine obtaining FDA approval to initiate the MOTUS IDE study and helped to earn the device its breakthrough designation.
“The main pain sources in the lumbar spine typically include the facet joints, compressed nerves, degenerated discs and some misalignment,” said Dr. Hodges, who serves as 3Spine’s Medical Director. “To maximize the benefits of surgery for patients, we needed to reconstruct all three columns of the lumbar spine.”
One significant challenge in this approach has always been accessing the posterior aspect of the interbody space, Dr. Hodges noted.
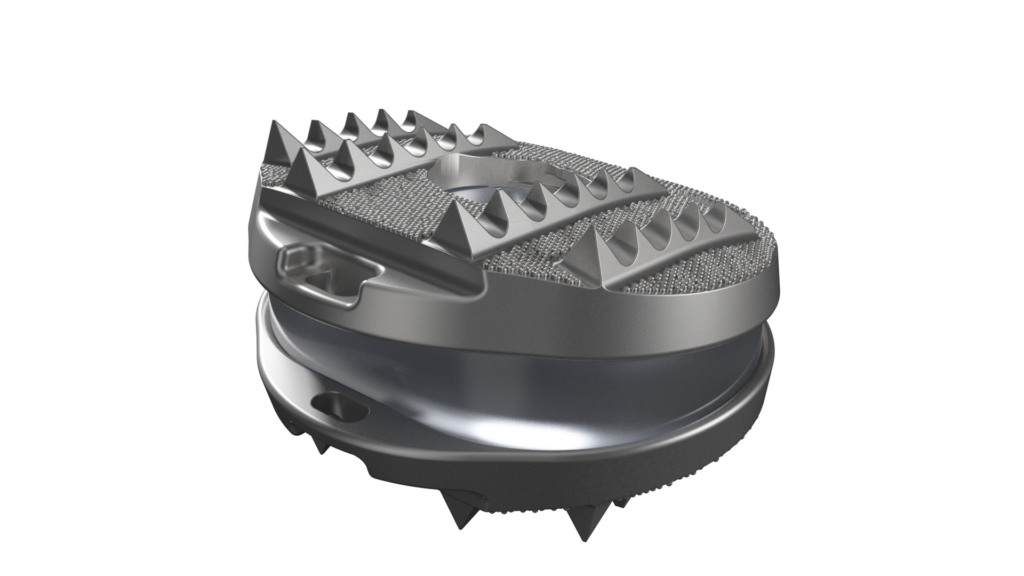
“The only viable method to gain this access involves completely removing both facet joints,” he explained. “After removing the facet joints, MOTUS restabilizes the spine and allows for motion to occur. The osteotomy is a crucial part of the surgery, allowing us to create an entry down the axis of both pedicles and insert the MOTUS device, which offers up to 18 degrees of motion.”
Dr. Hodges said 3Spine’s ultimate goal was to achieve spine stabilization and motion by using a wedge-shaped posterior column osteotomy. “This technique opens the posterior aspect of the interbody space, allowing for the insertion of a motion device that recreates stability and permits movement,” he explained. “For the implant to function properly, it must have a tail component, which provides the necessary initial fixation and stabilization.”
MOTUS is indicated for the biomechanical reconstruction and stabilization of a spinal segment after decompression at one lumbar level from L1/L2 to L5/S1. Surgeons implant the device through a posterior approach to replicate the function of the replaced disc and facet joints.
The device’s dual bearings resist motion and shear, and carry compressive axial loads like a native disc would. It is made of highly cross-linked antioxidant vitamin E polyethylene that is compression molded into a cobalt-chrome, titanium plasma sprayed substrate. Its articulating surface is made from highly cross-linked polyethylene that interacts with a cobalt-chrome end plate.
“The outcomes of current artificial disc replacement are extremely positive, but facet issues, stenosis and instability will continue to limit the procedure’s indications,” Dr. Hodges said. “Our solution’s big advantage comes from treating all pain generators and correcting segmental alignment issues.”
True change only comes once in a generation, said Pierce D. Nunley, M.D., Chairman of the American Board of Spine Surgery. “When I first saw MOTUS, it seemed too simple,” he added. “But in medicine, simple is best.”
He believes that the device has the potential to “fundamentally change spine care.”
MOTUS is the first of its kind, according to Jeffrey A. Goldstein, M.D., a principal investigator in the FDA clinical trial. He said 3Spine has developed something with “remarkable significance.”
Roughly 80% of Americans are likely to experience lower back problems, a factor that contributes to the estimated 500,000 lumbar spine procedures performed in the U.S. each year.
Dr. Hodges has encountered numerous patients in his practice who have undergone fusion surgery and experienced hyper-physiologic forces above or below the fusion site. This often necessitates revision surgeries, and after multiple revisions, these patients generally have a poor quality of life.
Clinical studies have demonstrated the importance of preserving motion in the lower back after surgery to allow patients a return to normal life activities. New motion-preserving techniques may achieve that aim in ways that fusion surgery cannot, and spine companies have taken notice.
Axiomed’s Freedom implant provides a viscoelastic disc replacement solution with natural spine motion.
Advances to Watch
The latest trends in motion preservation signal a promising future based on game-changing innovations and an important shift toward minimally invasive and biomechanically optimized surgical approaches that restore natural spinal function.
Ron Sacher, Founder and CEO of Premia Spine, noted that artificial facet replacement technology has been advancing rapidly in the past few years because of its potential for better patient outcomes. He said the technology allows surgeons to completely reimagine the way they treat patients.
Impliant began development of the TOPS System in 2003. Sacher purchased the company’s assets and formed Premia Spine in 2011. After decades of development and clinical studies, TOPS received FDA Premarket Approval in 2023.
“The traditional solution for lumbar spinal stenosis and spondylolisthesis is conservative care,” Sacher said. “If this fails and the disease state progresses, surgery is required. Until recently, patients had to choose between undergoing decompression or decompression with rigid fixation fusion. There was no middle ground. That changed with the introduction of facet replacement — the Goldilocks solution for spinal stenosis and spondylolisthesis.”
Facet replacement combines the advantages of fusion surgery (segmental stability) and decompression (maintained segmental motion), according to Sacher. He said that facet replacement allows surgeons to perform an optimal decompression of the impinged neural elements to achieve the best relief of pain symptoms and optimal improvement in joint function.
This is not possible with decompression or fusion surgery performed alone, Sacher noted. In the case of a decompression-only procedure, the surgeon must avoid over-decompressing the vertebrae. If they are too generous with the decompression, the patient is likely to return with a painful, destabilized segment that requires fusion. Conversely, if the surgeon doesn’t decompress the joint enough, the patient is unlikely to achieve maximum pain relief and a return to normal function.
Likewise, a surgeon who opts to fuse vertebrae joints needs to leave enough bone in place to create the biological bridge for the fusion to take hold and therefore might under-decompress the joint in the process. Further, morbidity associated with open and minimally invasive fusion — adjacent segment disease and new or worsening neurologic deficits — impact a large portion of these patients.
“With facet replacement, a surgeon can perform a bilateral facetectomy and laminectomy to remove all pain generators, and then stabilize the segment to recreate normal motion with an artificial facet joint in flexion, extension, rotation, bending and sagittal translation,” Sacher said.
In a key FDA study, Premia Spine’s motion-preserving TOPS System outperformed fusion in a head-to-head randomized prospective clinical trial. The results were so compelling that FDA granted TOPS a label of superiority to fusion, the first time a lumbar spine implant was granted such a claim. Overall, the study suggested that artificial facet replacement provides better post-op spine functionality, results in fewer revisions and better overall clinical outcomes and improves or prevents neurological deficits.
Spine companies continue to develop artificial disc technology using advanced materials such as metal alloys, ceramics and polymers that show improved durability, biocompatibility and wear resistance. Innovations in implant shape, size and articulation aim to restore normal spine motion while reducing stress on surrounding vertebrae to reduce the risk of adjacent segment degeneration.
Because of the increasing demand for disc replacements — and the willingness for payers to cover them — spine surgeons are investing in and adopting new systems to treat patients suffering from degenerative disc disease.
AxioMed seeks to develop the next generation of cervical and lumbar implants with its viscoelastic total disc replacement solution. The Freedom Cervical Disc is sold outside of the U.S. and the Freedom Lumbar Disc is in development.
Jeffrey Carlson, M.D., an orthopedic spine surgeon in Virginia, pointed to AxioMed’s single-piece design as a primary advantage of the device. He said the polymer core is what allows for the device’s natural motion and weight bearing that closely matches what the natural spine looks like and how it moves.
Mark McFarland, M.D., a Virginia-based spine specialist, said surgeons are looking for the holy grail of disc replacements — a device that mimics the human disc that it’s replacing. He said two- and three-piece implants on the market don’t achieve that goal because they are not compressible, unlike the AxioMed disc.
Centinel Spine provides alternative solutions to spinal fusions with its prodisc series. J. Alex Sielatycki, M.D., a spine surgeon at Steamboat Orthopedic & Spine Institute in Colorado, is one of the surgeons who has used the prodisc cervical system, noting that it’s well suited for cervical arthroplasty because of its wide range of implant options and customizability. He said this versatility allows surgeons to accommodate variations in endplate anatomy, bone quality and width with a single system.
DISC Surgery Center at Newport Beach is also looking closely at the efficacy of cervical disc placement in a two-level clinical study that kicked off last November. Specifically, the center is evaluating the effectiveness and safety of the Orthofix M6-C artificial cervical disc in patients who specifically have symptomatic cervical radiculopathy with or without cord compression. The results of the study are being compared with patients who undergo anterior cervical discectomy and fusion surgery.
What’s Next?
When it comes to surgeons actively using motion-preserving spine implants, their adoption boils down to effectiveness, which has a lot to do with the design of the devices and the materials that are used to construct them. There have been significant advancements in materials, constructs and implantation techniques that improve the form and function of the implants.
“The major advancement involves combining titanium alloy for structure integrity with polycarbonate urethane for durable cushion-bearing articulation,” Sacher said. “The integration of an encasement around the joints provides unimpeded movement of the internal articulating elements. The reliance on pedicle screws to affix the motion implant to the spine ensures that surgeons are familiar with the implantation technique and eliminates a learning curve.”
Advancement of motion preservation technologies and techniques will rely heavily on the benefits they can offer patients. As more is learned about how spinal fusions are linked with high reoperation rates, adjacent segment disease and other potentially problematic outcomes, greater attention will be paid to the development of disc, facet and total joint replacement devices.
As studies continue to demonstrate the efficacy of these implants, surgeons will be more interested in adopting the technologies and spine companies will be more inclined to invest in the development of advanced solutions. For patients, this could mean better pain relief and improvement of spine function.
Increasingly informed patients are becoming more interested in faster recovery times, something motion-preserving surgery can offer, depending on the patient’s age and health status.
Improved patient outcomes are a worthy goal but there’s financial payoff for companies that are willing to invest in the advancement of technology. ORTHOWORLD noted that motion preservation devices represents a $1.2 billion market opportunity on which companies have yet to capitalize. There’s no time like the present to catch up with 3Spine and Premia Spine, which have a 20-year head start.
NHM
Natalie Hope McDonald is a contributing editor.