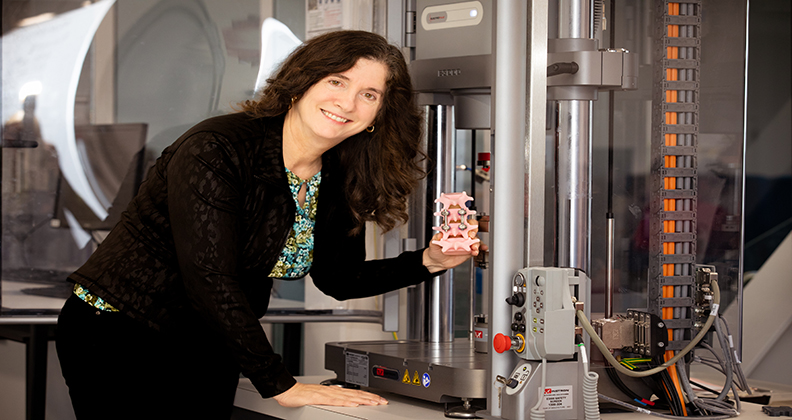
Deborah Munro, D.Eng., is nothing if not persistent. The medical device engineer turned academic turned entrepreneur has been working on ways to take the guesswork out of spinal fusions for more than two decades.
Her prototype sensor, which functions like a strain gauge, attaches to a rod that surgeons insert to measure the force exerted on the surface of fusion implants. She also invented a wireless sensor and software to interpret real-time data transmitted from the gauge, which helps to determine fusion success. The load measurement on the construct should be at its highest at the time of surgery and gradually decline over time as supportive bone ingrowth occurs.
“I’m looking for next-stage funding to support a full-scale animal study that will assess the biomechanics of the device and ensure that the stiffness of the fusion construct matches what the string sensor indicates,” said Dr. Munro, President of Munro Medical and Associate Professor in Mechanical Engineering at the University of Canterbury in New Zealand. “I’ll then be able to approach FDA with that proof to secure an Investigational Device Exemption and move forward with a human clinical trial.”
After a string of fits and starts, Dr. Munro is rounding the final bend of a circuitous and fortuitous product development pathway.
Inspiration Strikes
Dr. Munro developed a level of frustration at the glacial pace of innovation in orthopedics while working as an engineering manager at Synvasive in the late nineties. She decided to take steps to make the change she wanted to see happen by pursuing a Doctor of Engineering degree at the University of California, Davis.
It was there that she crossed paths with Munish Gupta, M.D., the Chief Surgeon at UC Davis Medical Center who performed complex reconstructive spine surgery. Dr. Gupta told Dr. Munro about the challenges of determining the success of the spinal fusions he performed.
The success rate of spinal fusion surgery is lower than other orthopedic procedures and the ability to predict fusion outcomes is inherently unreliable, according to Dr. Munro. She said surgeons typically review x-rays six weeks after surgery to check for evident issues at the fusion site, then schedule another round of imaging at the three-month mark to check again.
“However, these early x-rays don’t provide significant information about fusion success,” Dr. Munro explained. “It often takes four to six months for indications to become apparent that allow surgeons to make judgment calls.”
With no conclusive way to know whether spine fusions take, Dr. Munro said, surgeons tend to be conservative in how long they wait to determine the success or failure of the surgery. Recovering from spinal fusion therefore requires weeks of bed rest.
Dr. Gupta asked Dr. Munro: Is there a more effective way to determine the success of spine fusion? Why should outcomes be based on surgeons’ subjective views of x-rays taken weeks after surgery?
He referred her to a study published in The Journal of Bone and Joint Surgery that explored the biomechanical, radiographic and histological properties of posterolateral spinal fusion in sheep models to assess changes in the load-sharing of implants and fusion mass throughout the healing process. Surgeons involved in the research assessed the quality of the fusions. According to the study, it took four months for the surgeons to achieve unanimous agreement on the failure or success of the surgery.
“Surgeons generally aren’t aware that fusions fail until three to four months post-op,” Dr. Munro said. “At that point, they perform a second highly invasive procedure to re-fuse the vertebrae and more bone is harvested from the pelvis and spread over the spine to stimulate bone growth, which creates the fusion.”
Dr. Munro knew that wasn’t an ideal approach to patient care. She also knew how to go about finding a better solution.
Developing the Solution
Dr. Munro’s mechanical engineering background allowed her to break down spine fusion constructs into basic terms: a round beam with screws on either side that offer simple support. She knew that placing a strain gauge in the middle of the construct’s span along the outside fibers would measure where maximum strain occurs on a simply supported beam under a bending moment.
“This placement allows for the tracking of load-sharing dynamics until full strength of the fusion is achieved, which is indicated by a strain plateau,” Dr. Munro said.
The sensor could also provide surgeons with real-time information about the strength of a fusion. “When the sensor is first implanted, it should display the maximum strain,” Dr. Munro said. “Otherwise, the surgeon knows the fusion didn’t work, perhaps because of tiny cracks in the implant, broken pedicle screws or loose rods — things that are invisible to the naked eye. This immediate feedback allows surgeons to address the issues during the procedure.”
Dr. Munro, who subscribes to Murphy’s Law, had to consider the safety profile of her implantable device. She avoided using biotoxin materials, and all connections in the device are made of materials like gold and titanium that are inert in the body. The device doesn’t contain separate components that are susceptible to breakage or loosening, which minimizes the risk of patient harm.
Although the concept of wireless power existed when Dr. Munro was developing her prototype, it hadn’t been applied to medical implants.
“It was challenging to figure out how to transmit electromagnetic energy to the device through human tissue,” Dr. Munro said.
She took classes in nanotechnology, bioinstrumentation and electrical engineering and eventually joined the faculty at the University of Canterbury, where she had the support and resources needed to devise a wireless sensor that runs without batteries.
Preliminary lab testing of Dr. Munro’s device has shown promising results. She recently received seed money to evaluate the transmission of electromagnetic energy to the device in an animal model, marking a significant milestone in the product’s progression.
Market validation studies involving consulting surgeons, including Dr. Gupta, suggest the device shows promise for improving spine fusion outcomes and reducing disability, bedrest duration and core muscle atrophy for patients.
Quicker postoperative mobilization could enhance the strength of fusions and speed recovery times, according to Dr. Munro. After countless hours of challenging work, out-of-the-box thinking and stick-to-itiveness, she is close to achieving what she set out to do more than twenty years ago. It’s been time well spent.
DC
Dan Cook is a Senior Editor at ORTHOWORLD. He develops content focused on important industry trends, top thought leaders and innovative technologies.




