Albert DaCosta co-founded Paragon 28 to turn the foot and ankle segment on its head instead of merely participating in it. “Our mission is to improve outcomes and really put a mark on the market,” said DaCosta, the company’s CEO.
That’s no small feat when you consider the complexity of the procedures that trauma surgeons perform. “The foot and ankle environment is a marvel when you start to appreciate the number of bones and the interactions of those bones with soft tissues,” DaCosta said.
The overall growth of the foot and ankle subsegment has buoyed the trauma market, which saw a normalization of procedure volumes in 2023 and is expected to reach $9 billion in sales this year.
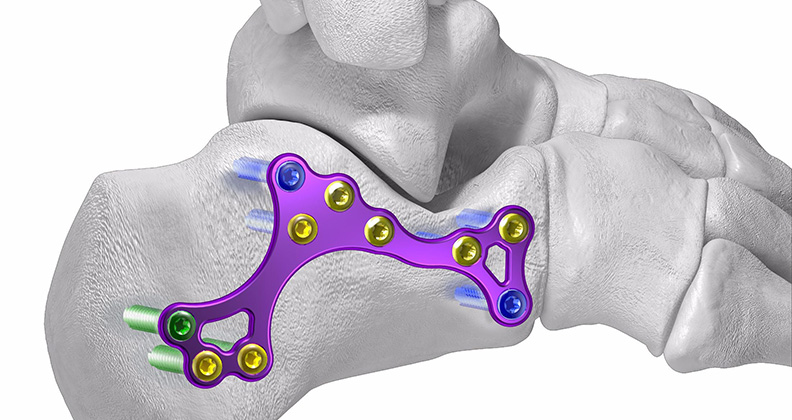
Paragon 28’s efforts are part of a larger movement within foot and ankle, as companies pump resources into the development of implants made of advanced materials that fit precisely into complex anatomy and support bones and tendons without damaging surrounding soft tissue.
Up for the Challenge
DaCosta said Paragon 28’s strategy for implant fixation involves balancing material properties with anatomical considerations. “It’s a combination of implant design and soft tissue performance,” he added. “For certain ankle fracture patterns we might use a titanium plate, and in these cases, we prefer lower-profile products that offer the ideal balance of strength.”
Paragon28’s product line includes a mix of materials such as PEEK, titanium and stainless steel. According to DaCosta, the company’s products are continually evolving, driven by an R&D team that carefully selects materials that are used to achieve the ideal balance of performance. He emphasized that Paragon 28 is focused on enhancing the precision of the bone-to-metal interface.
“We view this precision as a biological stimulus,” he explained. “We are careful not to use materials that might inadvertently damage the delicate branches of bone and always pay close attention to the accuracy of our drilling and metal interfaces.”
Using PEEK as an example, DaCosta explained that Paragon’s R&D team carefully evaluates the benefits and drawbacks of implant material when developing new products. “We know that one limitation of PEEK is that bone doesn’t readily attach to it, leading the body to form a fibrous film around the implant,” he said. This fibrous film can reduce pressure on the surrounding bone, causing destabilization and other complications.
According to DaCosta, a low-profile design improves load distribution and reduces soft tissue irritation during healing. He acknowledged that replicating the complex anatomical structures around the ankle is a significant challenge, but one his company is eager to tackle.
“For ankle fractures, we prefer suture-based products that provide some stress relief while still allowing for recovery,” he said. “We’re working to match the intricate anatomy and soft tissue structures of the ankle and make the materials work to our advantage.”
As an example, DaCosta highlighted the need for precisely designed implants to treat ankle injuries, citing partial anterior inferior tibiofibular ligament tears. “It’s one of the soft tissue structures around the ankle, and we’re talking about a millimeter to repair,” he said.
Blood supply plays a critical role in bone quality, which DaCosta said is a major factor in foot and ankle implant design. “The further you are from the heart, the weaker the blood supply — toes have some of the weakest circulation,” he explained. “As a result, bones in those areas are less likely to heal effectively.”
If screw heads aren’t “aggressively sharp,” according to DaCosta, they can fracture the delicate branches of trabecular bone that are crucial for stable fixation. “It’s similar to using a sharp knife versus a dull one,” he explained. “The right pitch and separation of threads can enhance precision between bone and metal, improving outcomes in areas where bone quality is already compromised.”
Part of Paragon 28’s trauma product line is specifically designed for patients with chronic bone conditions. For example, patients with Charcot foot are often morbidly obese and neuropathic, with many unable to feel their extremities. “Over time, the bone degrades to the point where it loses much of its structural integrity,” DaCosta said. “If we create implants that are too rigid or strong for these patients, the screws or plates can cut through the bone.”
To address this risk, Paragon 28 designs surgical techniques that apply strong compression during installation and utilize materials that remain flexible throughout the implant’s lifespan.
DaCosta believes that increased attention to soft tissue considerations will play a key role in the future of trauma implant design. “Bone deformities show up on x-rays and CT scans, making it easy to link deformities to bone structures,” he explained. “But what is often overlooked is the surrounding soft tissue — that’s the challenging part to visualize. It’s even difficult to accurately measure the accumulation of soft tissue layers.”
DaCosta predicts that as understanding of soft tissues advances, tools like artificial intelligence will help develop more sophisticated algorithms tailored to specific stages of fractures and deformities. These tools will provide surgeons with insights into the condition of surrounding tissues, allowing them to make more precise corrections while balancing soft tissue and bone dynamics.
“I think there’s a lot of progress to be made, and as we become better at tracking the successes and failures of implant performance, it will lead to significantly improved surgical outcomes,” he said.
Additive Advancement
Vadim Gurevich, President and CEO of GLW Medical Innovation, highlighted the way the company combines traditional implant materials with advanced manufacturing techniques to create foot and ankle implants that are more user-friendly for orthopedic surgeons. “We use 3D printing to manufacture our plates, then inject PEEK beneath them to create a unique platform that allows for increased visibility in the operative field,” Gurevich said.
The key advantage of this see-through technology is that it provides surgeons with immediate visual clarity in the operating room. Although enabling technologies like robotics and AI-assisted navigation tools have been shown to enhance surgical precision in spine and joint replacement surgeries, Gurevich said these tools are not yet designed to handle the inherent complexity of foot and ankle procedures.
“In trauma surgery, enabling technology isn’t always applicable,” he explained. “Robot assistance isn’t available because robots require consistent, repeatable steps.”
Given the visualization challenges that foot and ankle surgeons face, GLW Medical is stepping in with a valuable solution. Additionally, the rise in periprosthetic surgeries, driven by an aging population, further underscores the need for advanced visualization tools.
For these reasons, Gurevich said, 3D printing has a future in large-scale foot and ankle applications. While personalized, additively manufactured implants remain relatively expensive, GLW Medical is implementing additive manufacturing at scale. Gurevich envisions a future in which more companies explore the use of biomaterials for trauma implants, and hospitals use 3D printers to assist with temporary fixation for trauma patients.
“The challenge is that no biomaterial has so far matched the strength of titanium,” he said. “Until one does, we need to rely on titanium to produce implants.”
Despite seeing opportunities for innovation in foot and ankle implants, Gurevich believes that competing interests are creating a landscape that hinders progress. “The focus is no longer strictly on innovation,” he said. “It’s also about the cost of innovation.”
According to Gurevich, orthopedic companies frequently launch new products that feature only minor, incremental improvements. He said companies aim to maintain price points that are appealing to healthcare facilities, but value analysis committees are pushing back, claiming that companies aren’t offering products that provide significant benefits to currently available options.
“As a result, the emphasis on innovation needs to shift,” Gurevich said. “It should be directed toward manufacturing efficiency — not necessarily in developing new materials, but in finding ways to make implants more cost-effectively.”
PM
Patrick McGuire is a BONEZONE Contributor.




