Advancing surface technology is crucial to the development of orthopedic implants that last longer and help to prevent postoperative infections that are increasing in number. Figuring out which improvements to prioritize and how to allocate R&D funds toward them is a bit more complicated.
Brandon Miller, Business Development Manager at Lincotek Medical, believes those concerns can be addressed by answering three key questions.
“If you can say yes to any of these questions, you’ve got a good product,” he said. “If you can answer yes to two, you’ve got a great product. And if you can affirmatively answer all three, you’ve hit a home run with a product that can capture significant market share.”
Does it Improve Patient Outcomes?
Orthopedic OEMs and suppliers, like Lincotek, are exploring surface technologies that impact infection control, bone ingrowth, bone incorporation and implant durability to improve patient outcomes. Lincotek is also actively evaluating nano surfaces as more patients present for surgery with higher rates of diabetes, elevated BMIs and increased use of narcotics and steroids —comorbidities that lead to higher postoperative infection rates.
“We believe some of the anti-bacterial nano surfaces on the market today offer substantial value,” Miller said. “Some of these surfaces are bioactive, incorporating hydroxyapatite (HA) components, which promote bone incorporation and may also offer prophylactic infection prevention.”
Another key area of focus among orthopedic companies is improving long-term implant durability, which involves developing enhanced articulating surfaces for total joint implants.
“We’ve seen promising preliminary results with new materials, and one notable trend is the decreasing reliance on cobalt chrome,” Miller said.
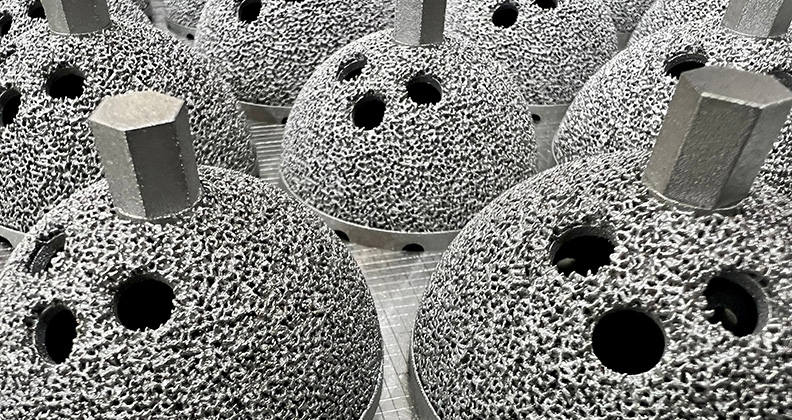
To promote bony ingrowth, one of the major factors in preventing early implant failure, Lincotek is exploring the development of an additive-manufactured porous structure that’s designed to mimic native bone.
When Miller began in the industry in 1997, orthopedic surgeons used cancellous bone autografts or synthetic porous grafts, packing them into the graft site. They’d sometimes combine the two types of products to achieve greater volume.
Additive manufacturing can now be used to create a structure or lattice that fosters an excellent cellular environment for bone growth, Miller noted. He said mesenchymal stem cells, osteoblasts and osteoclasts thrive, reducing the risk of early implant failure in total joint replacement patients.
“When combined with a hydroxyapatite (HA) nano-surface, the implant not only promotes bony incorporation but may even help prevent infection,” he said.
Does it Make the Surgeon’s Job Easier?
Lincotek has gone beyond anodizing pedicle screws to working with anodized surfaces on additive-manufactured implants. The company is focused on reducing contaminants and ensuring that implants are extremely clean and visually polished with consistent coloring across surfaces.
When Miller first started covering cases in a sales role for Zimmer Biomet and for the first 10 to 12 years he spent in the industry, surgeons worked with the same first assistant, scrub tech and circulating nurse during each case. Now, he said, surgeons might work with a cardiothoracic first assistant who isn’t as well versed in orthopedic instrumentation.
The anodizing process helps to make life easier for the surgical team by simplifying the setup for surgical procedures. After making the initial incision and assessing the surgical field, a surgeon can alert team members that they’ll be using 8mm instruments during the case and instruct them to pull and open all “green” tools.
“This reduces operative times, decreases the likelihood of infection and lowers surgical costs,” Miller said.
Does it Save Money?
Miller noted that developing breakthrough nano-structured technologies will require more cooperation from FDA.
“We need expanded indications that allow us to bring new products to market under 510(k) clearances rather than relying on lengthy and costly IDE trials, which can take up to five years and as much as $100 million to complete. That’s a level of risk that many orthopedic manufacturing companies cannot tolerate.”
Miller added that the push for better solutions is often stalled by high regulatory and development costs for new materials and places a premium on investing in surface technologies. He said Lincotek is increasingly looking at ways to combine new technologies rather than developing separate products and gaining FDA clearance for each.
For instance, he said, integrating a DLC surface onto an additively manufactured part can streamline manufacturing processes and achieve a quicker return on investment.
“When evaluating new material technologies, industry can’t focus solely on durability and surface smoothness,” Miller said. “It also needs to ensure that the manufacturing process is efficient. Companies must minimize scrap, contain costs and ensure biocompatibility while maintaining the quality of the surface technology.”
Miller acknowledged a common misconception about additive manufacturing throughout the orthopedic industry: Many OEMs believe it’s simply about printing an existing design faster and cheaper.
“However,” he said, “it’s important to emphasize the need for additive design and manufacturing to develop better implants. If an implant isn’t superior in its design, there’s no point in printing it. We want to push the boundaries within the 510(k) framework by creating porous structures that promote additional bone growth and offer improved patient outcomes.”
Lincotek focuses on the regulatory process as a starting point and prioritizes obtaining 510(k) clearance rather than tackling an IDE. “Having managed multiple IDEs, we know it’s not always a feasible path,” Miller said.
Miller highlighted the importance of a proven quality management system that integrates seamlessly with OEM customers. He also noted that in-house material scientists and engineers must work closely together.
“Manufacturing engineering must be integrated into this process to maintain cost control and produce high-quality products that meet diverse needs,” Miller said.
Miller pointed out that saving money doesn’t always involve reducing the cost of implants. “It can also result in minimizing the need for revision surgery, reducing the need for a second surgery or creating a longer-lasting product that lowers overall healthcare costs,” he said.
DC
Dan Cook is a Senior Editor at ORTHOWORLD. He develops content focused on important industry trends, top thought leaders and innovative technologies.




