
Fracture care is quickly evolving past the set-it-and-forget-it approach as casts and splints have been replaced with plates and screws. Although the development of most fracture repair technologies focuses on engineering implants to heal bones, others are looking to injectable bioadhesives to stimulate bone healing.
Fracture repair devices and instrumentation are also changing to adapt to evolving minimally invasive surgical techniques and advancing technologies that are quickly becoming mainstays in orthopedic operating rooms.
Starr Frame offers platforms for the closed reduction of significantly displaced pelvic rings and acetabular fractures. The company’s flagship product, which shares the same name as the company, has been on the market for 10 years and was designed to assist surgeons through a minimally invasive step-by-step approach that results in gradual and precise correction of bone deformities and reduced surgical times.
The company recently launched an updated version of the product, the Starr Frame Orion, with one major adjustment.
“The original Starr Frame, which is still on the market, has vertical carbon fiber frame halves that attach to each side of the operating table, and attached to those frame halves are a series of instruments and pins that are used in the reduction surgery,” said Starr Frame Managing Partner Robert Sudol. “With the Orion, those frames are now curved and meet over the top of the operating table instead of on each side.”
The reason for the change, Sudol explained, is that some new surgical navigation imaging systems feature smaller apertures and cannot adapt to the original product’s vertical constructs. With its lower curved profile, Starr Frame Orion is designed to accommodate imaging systems with no issue. The product’s update reveals the growing influence that intraoperative imaging technology now has on the way that fracture repair surgery is performed.
Another emerging trend in fracture repair is the adaptation of existing technologies to treat complex conditions that cannot be addressed with conventional device solutions.
The Bone Bolt System — developed by the Louis S. Peery, M.D. Orthopaedic Innovation Center (OIC), a collaborative effort between the Department of Orthopaedics and PIVOT Center at the University of Utah — is designed to treat complex bone breaks, such as pelvic fractures and those of the long bones in the arm and leg.
“Like a lot of new products, the Bone Bolt System is based on an unmet clinical need, which in this case is addressing fragility fractures and bone that’s osteopenic and osteoporotic,” said Wade Fallin, Research Professor in the orthopedic department at the University of Utah and Executive Director of OIC. “In situations where standard cannulated screws don’t have sufficient strength to repair fractures, the Bone Bolt is a device that provides much greater fixation strength and much greater stability than a similar-sized screw.”
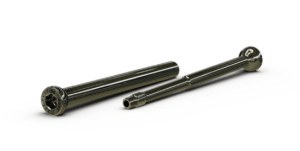
The Bone Bolt System is a novel implant designed and developed for percutaneous bone fracture fixation.
Bone Bolt was recently cleared to market by FDA and is primarily designed to treat patients with compromised bone quality. Fallin explained that the platform can also be applied during arthrodesis or osteotomies — essentially any time two or more bone fragments need to be repaired.
Fallin said that the weak link in a standard cannulated screw is its threads, which can lose fixation within bone, resulting in the loss of implant stability. “Bone Bolt solves that weakness by including a screw head on either side of the construct, and it does this through two interconnecting pieces with a head on either side,” he said.
Designed and developed for percutaneous bone fracture fixation, Bone Bolt embraces the larger trend of using smaller implants and minimally invasive surgical methods for fracture repair. According to Fallin, OIC is currently developing numerous fracture repair devices, including a next-generation bone screw.
“Instead of being a passive bone screw, it maintains dynamic compression at the fracture side of the repair as the bone fragments settle and remodel,” Fallin said. “We know from non-unions and other failures of bone healing that maintaining compression at the bone healing site is critical to ensure a successful repair.”
Fallin highlighted Conventus Flower Orthopedics’ FlexThread Intramedullary Nail as an innovative device that’s delivering significant advantages to the treatment of fractures in patients with compromised bone quality. “Instead of fixing the fracture with a bone plate and bone screws, surgeons repair it from the inside with an intramedullary device, which is much stronger and far less invasive,” he explained.
FlexThread technology allows the nail shaft to flex upon insertion and then self-contour to native anatomy. Its screw-like design simultaneously maintains fracture reduction while optimizing the bone purchase within the medullary canal.
Adaptable and Versatile
Some new fracture repair devices address not only the primary fracture but also the potential for more injuries that may occur at the same site. Meduloc is an orthopedic company that’s developing minimally invasive intramedullary implants for the treatment of various types of small and long-bone fractures. The company’s nitinol implants are known for their unique elastic properties and can revert to their original shapes after being bent.
When patients suffer a boxer’s fracture, the most common type of hand fracture, they break the fifth metacarpal bone.
“Surgeons typically place a screw down the middle of the fracture, which has become the preferred repair technique,” explained Joshua Hustedt, M.D., M.H.S., an orthopedic surgeon and Meduloc’s Medical Director and Co-Founder. “The screw can bend if the patient punches another object. The injury then becomes very difficult to manage.”
To remove and replace the bent screw, Dr. Hustedt said, surgeons must re-break the bone during a challenging procedure that causes further injury to patients.
Despite the popularity of intramedullary screws in fracture repair, Dr. Hustedt said that many surgeons warn against their use for patients who suffer a boxer’s fracture because of the difficulty in treating the initial break if the screw is bent after another injury.
Meduloc’s metacarpal intramedullary fixation device is designed to return to its original form after bending if a patient re-breaks the bone at the same site. According to Dr. Hustedt, the technology self-reduces the fracture because the nitinol-based implant is designed to bend with the refracture and then “pop” straight again.
“When we design devices, we have to treat the patient — you can’t just treat the fracture,” he said. “A lot of patients with a boxer’s fracture are likely to suffer the same injury, so we tried to come up with a solution that treated the fracture, but also treated the patient.”
While Meduloc’s technology was originally developed specifically for the metacarpal, Dr. Hustedt believes it can deliver different indications, improvements and benefits for other areas of the body. With this philosophy in mind, the company is identifying unmet clinical needs in other applications for which their technology could be useful, including for the treatment of clavicle and ankle fractures.
The Pangea Plating system, which received FDA 510(k) clearance in September 2023, includes applications for fractures in the femur, fibula, tibia, humerus and utility, and is expected to be Stryker’s largest-ever trauma product launch. The system was developed using the Stryker Orthopaedic Modeling and Analytics (SOMA) program, which collects CT scans from hospitals and institutions from across the world.
“The collection of CT scans are segmented in a standardized manner as 3D bone models and stored in a database with patient demographic data,” said Eric Tamweber, Vice President and General Manager of Stryker’s trauma business.
The data was mined by algorithmic applications to deliver specific anatomical and demographic insights that informed the design of the Pangea systems. The collaborative efforts of 26 world-renowned orthopedic surgeons were also key in developing the plating platform.
Armed with a vast library of anatomical information, Pangea Systems is a portfolio of anatomically informed implants aimed at improving fit for a diverse patient population. The platform spans six indications and provides variable angle locking throughout the entire portfolio of anatomic and utility plates.
“Pangea includes 33 plates, which differentiate us from the competition,” Tamweber said. He added that the system will become Stryker Trauma’s core plating brand and will continue to expand in the future.
According to Tamweber, the plating system’s variable angle locking technology employs a cobalt chrome screw within the titanium alloy plate. “It allows the screwhead’s threads to form a definitive plate/screw interface in the plate’s locking hole by engaging the softer titanium alloy,” he explained. “Based on the mechanical properties of the two different types of metals, the cobalt chrome locking screws will not cold weld into the titanium plates.”
A simple design concept and ease of use within hospitals were another major focus in the development of the Pangea Systems, explained Tamweber. He said staffing constraints and limited inventory space at surgical facilities, including ASCs, inspired the streamlined design of the systems, which come packaged in just two trays.
Increased Healing Power
BONESUPPORT’s CERAMENT G is a combination matrix comprising a resorbable synthetic bone graft substitute and the antibiotic gentamicin. The bone graft substitute fills gaps and voids in bone to promote healing and prevent bone infections. It can also augment the effectiveness of implants and bone alignments, according to the company.
Last March, CERAMENT G received FDA 510(K) clearance for use in open fractures, an indication that more than doubles the accessible market in the U.S. The clearance should contribute to BONESUPPORT’s continued growth.
CERAMENT G was a significant factor in the 104% increase in North American sales the company realized in 2023.
“Open fractures are one of the most common causes of a patient developing a bone infection, and we are very excited about this expanded indication,” said Emil Billbäck, CEO of BONESUPPORT. “It means that American surgeons will have a new powerful tool to treat patients with skeletal injuries while simultaneously protecting the site from infection by local elution of antibiotics.”
PBC BioMed has developed OsStic Synthetic Injectable Bone Void Filler, a structurally and mechanically enhanced bioadhesive for reduction, provisional fixation or void-filling of peri-articular fractures and defects. The filler enhances structural stability where standard fixation alone cannot provide sufficient support for functional mobilization.
“This indication does not currently exist for any other biomaterial on the market today,” said Gerard Insley, Ph.D., Chief Scientific Officer at PBC BioMed. “That’s why it received Breakthrough Device Designation from FDA in January.”
OsStic is a calcium-based cement that contains phosphoserine, a phosphorylated amino acid. “The phosphoserine molecule enhances the mechanical strength of the calcium phosphate cement to levels that are significantly above standard calcium cements on the market,” Dr. Insley explained. “This makes the material potentially suitable for enhancing the structural stability of standard fixation during fracture repair.”
He pointed out that preclinical trials indicate that the calcium phosphate-based adhesive properties of OsStic also facilitate cell-mediated remodeling that may allow for more natural healing of fractures. He also noted that clinical trials demonstrate that the technology may allow patients to rehabilitate quicker through earlier functional mobilization.
Dr. Insley said the current standard practice of fixating fractures with metal implants is problematic in compromised bone. He believes combining implants with a suitable biomaterial could enhance the effectiveness of fixation devices while maintaining bone integrity.
The growing incidence of fractures in compromised bone is among the biggest challenges in trauma care.
“This is an opportunity for all innovators in the space to design solutions that enhance healing in these cases and improve patient outcomes,” Dr. Insley said. “Biologics such as growth factors and stem cells have promised much but delivered less. Many factors are at play, including technical complexity, regulatory hurdles and economics. Clinicians and patients have yet to see the benefits of the technology.”
PBC BioMed is investing significant resources into improving hardware stability, enhanced fixation, natural bone healing and preservation of as much natural tissue as possible at the fracture site, according to Dr. Insley.
“Our company is focused on a biomimetic approach that enhances the healing process, and we’re very hopeful this will lead to better outcomes and improved quality of life for patients,” he said.
PM
Patrick McGuire is a BONEZONE Contributor.




