In 2022, when college basketball teams from across the Midwest gathered in Sioux Falls, South Dakota, for the Summit League Tournament Championship, Nathan Skelley, M.D. was on hand to lend his expertise in case a player went down with an injury. The Sanford Health sports medicine surgeon was in a great mood as he soaked in the festive vibes of March Madness.
Then his cellphone rang with a video call. Dr. Skelley’s friend and former colleague, a general surgeon of Ukrainian descent, reached out with an urgent request for medical supplies that were needed in his homeland, which had recently come under Russian attack.
“That moment was surreal for me,” Dr. Skelley said. “While I was enjoying the excitement of the basketball games, lives were being torn apart on the other side of the world.”
It was a snap back to reality and a call to action that Dr. Skelley couldn’t ignore.
“I talked to the orthopedic team at Sanford Health, and we quickly offered the health system’s excess medical supplies,” he said. “My friend was very grateful for the help, but during follow-up discussions he specifically mentioned the dire need for external fixators to treat fractures in injured civilians and soldiers on both sides of the conflict.”
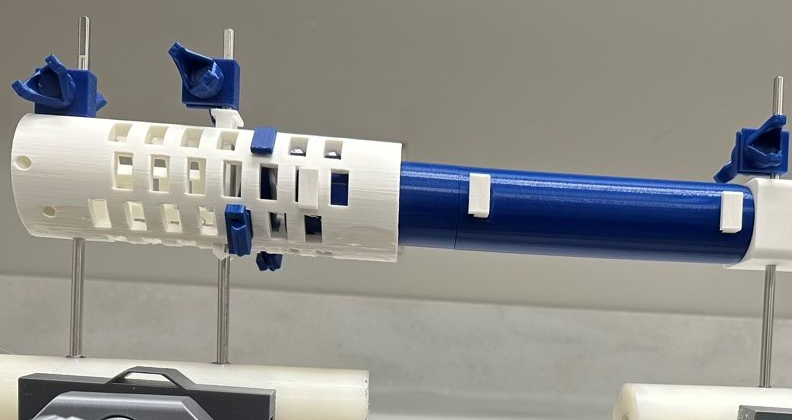
External fixators are complex pieces of medical equipment that stabilize limbs after high-energy trauma. The temporary devices are fixed into bones through metal pins to stabilize the injury and make the patient more comfortable until their fractures heal or they can receive further medical care. Dr. Skelley began to think about scaling the production of cost-effective devices that could be shipped to Ukraine and other areas of need throughout the world.
Searching for a Solution
As Dr. Skelley ramped up efforts to help people without access to advanced orthopedic care, he learned that SIGN Fracture Care International, a humanitarian organization based in the state of Washington, was already sending medical devices to war-torn Ukraine and many other medically underserved areas of the globe. When he reached out to better understand how he could help, representatives from SIGN said they were also working to obtain more external fixators for fracture care.
Dr. Skelley recognized the opportunity at hand and reached out to his colleagues throughout the Sanford Health System. He challenged the nearly 60 orthopedic surgeons to come up with a creative way to produce an affordable and effective device that would work as an external fixator.
“I received various hand-sketched ideas, including suggestions for using broomsticks, PVC pipe and duct tape,” he said. “Some concepts had great potential, but they faced scalability and supply chain resource issues.”
Dr. Skelley’s research at Sanford Health focuses on additive manufacturing applications in orthopedics, so he thought about designing a low-cost 3D-printed device that met the essential mechanical requirements of a traditional external fixator made of carbon fiber or stainless steel: maintaining fracture length, preventing bending and resisting rotation forces.
His colleagues were skeptical that a 3D-printed plastic device would work effectively, but Dr. Skelley was undeterred and got to work, using computer-aided design (CAD) methods to create and manipulate device iterations. Dr. Skelley, who has no engineering background, relied on numerous YouTube tutorials to teach himself how to use CAD software and turn his ideas into tangible designs.
He experimented with various bolt configurations and interlocking segments before landing on the concept of telescoping cylinders. Surgeons can use these cylinders to set the appropriate length of the fixation device. De-rotation and traction wedges with securing clips are hammered into place through windows on a honeycomb cylinder, which surrounds the distal aspect of the main rod construct.
The overlapping windows allow for numerous wedge placements at 2mm increments. The device’s size can be reduced or increased before 3D printing to accommodate fractures and patients of various sizes.
Dr. Skelley continued to refine and modify the device before conducting a pilot test at the Sanford Health – University of South Dakota Medical Center. The test results were published in the Journal of 3D Printing and Medicine.
Small and large components of the device can be produced on the same print bed in slightly less than two days. Dr. Skelley noted that about 10 external fixators can be made in a month using a single standard desktop 3D printer and then stored until they’re needed. The device’s compact size makes it feasible to send the potentially life-saving tool to areas in need.
“It’s a solution that can be distributed at critical times, such as responding to an earthquake in Haiti, civil war in Africa or the crisis in Israel and Palestine,” Dr. Skelley said.
Dr. Skelley approached Viaflex, a manufacturing and engineering company in Sioux Falls, to conduct independent mechanical testing on the device. The firm’s team of expert engineers smiled politely at his rudimentary CAD designs and got to work with testing. They were very surprised at how well Dr. Skelley’s device performed compared to standard medical-grade fixators. Dr. Skelley is submitting their findings for peer review and expects the results to be published before the end of the year.
“Printing these medical devices with desktop 3D printers is revolutionary and solves many production and distribution challenges,” he said. “If we can meet the necessary clinical and mechanical standards with this device, anyone with access to an approved desktop 3D printer and appropriate filament could create it. With the appropriate regulatory and safety approval, they could use our master file to manufacture these humanitarian aid devices for fracture care around the world.”

A deconstructed external fixator fits easily within a filament box for efficient storage and shipping.
Focused on the Bigger Picture
Dr. Skelley is not interested in commercializing the device. “My primary objective is to share the idea and concept, ensuring it reaches institutions equipped to carry out further comprehensive studies and clinical assessments,” he said. “The design thrives on being low-cost, rapidly producible and open source. I’m confident that the engineers and specialists at Viaflex, the University of South Dakota and other research institutions can make better and more efficient versions of my design.”
He’s releasing the device to the 3D printing community at large with the hope that experts take the design to the next level. “The open-source and collaborative nature of 3D printing allows for idea exchange and innovation,” he said. “Individuals with advanced design skills can enhance the device, ensuring it better serves those in need.”
Dr. Skelley has also been in discussions with SIGN to expedite the development and production of the device and distribute it across the group’s global network of humanitarian missions. He believes the significance of his project extends beyond the device itself. It represents the ways 3D printing can democratize access to medical equipment, enabling people worldwide to produce devices that make a significant difference in patient care.
“Our mission is to address the immense burden of musculoskeletal injuries, a global epidemic that often goes unnoticed in comparison to other medical conditions,” Dr. Skelley said. “While the world’s attention is understandably focused on infectious diseases and major health issues such as cancer and heart disease, the musculoskeletal burden is often underestimated and underappreciated.
“When an individual sustains a fracture in a long bone, their ability to care for themselves, work in their community or provide for their family is severely compromised,” he continued. “This has significant downstream ramifications for the entire region. Restoring a person’s musculoskeletal function allows them to return to routine life activities and work in their community.”
Dr. Skelley is passionate about his work and would feel immense gratification if surgeons around the world were able to use his device, or a variation of it, to assist patients in need. “It would truly be a source of profound satisfaction for our entire research team, to know that it made a meaningful difference in people’s lives that otherwise would not have access to advanced orthopedic care,” he said.
DC
Dan Cook is a Senior Editor at ORTHOWORLD. He develops content focused on important industry trends, top thought leaders and innovative technologies.




