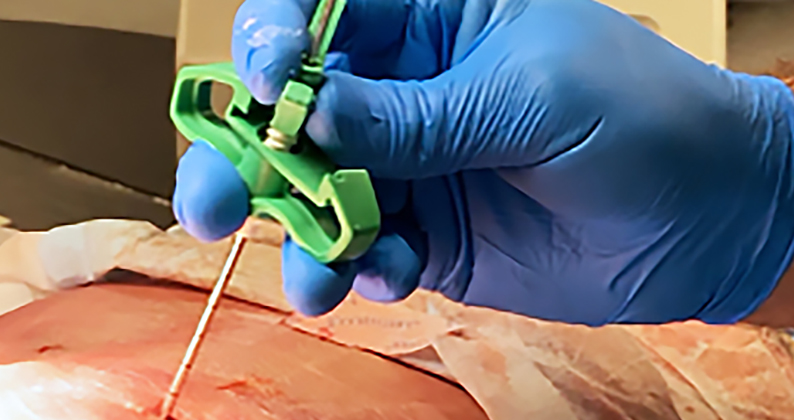
At Swedish Medical Center in Englewood, Colorado, minimally invasive procedures are used to treat fractures in the most cutting-edge way. Steven Morgan, M.D., an orthopedic trauma surgeon, places a revolutionary implant inside broken bones to expedite healing and add strength to the repair, particularly in higher-risk patients who might not tolerate open surgeries involving hardware fixation.
The IlluminOss System is injected in liquid form and conforms to the bone before light therapy is used to cure the liquid, turning it into a solid that stabilizes the fracture during a considerably shortened recovery process. Most notably, the implant material allows for more individualized treatment by molding to a patient’s unique anatomy.
Dr. Morgan said patients with lower extremity fractures can bear weight soon after the procedure to avoid the prolonged use of walking aids. “This new system augments a patient’s poor bone quality to increase its tolerance to the stress of early mobilization,” he explained.
The implant provides a potentially life-changing alternative for treating fractures in older individuals and patients who have comorbidities that make recoveries challenging and ambulation critically important.
It’s proving to be especially beneficial for osteoporotic patients 60 years and older. “A broken bone in a mature adult can be catastrophic,” Dr. Morgan said. “One study showed that fractures increase the risk of death for 10 years in patients older than 50.”
With so much at stake, trauma surgeons are increasingly employing arthroscopic surgery and percutaneous fixation to treat fractures. Patients are benefiting from much smaller incisions, reduced soft tissue damage and faster recovery times.
Minimally invasive treatments are just one aspect of exciting developments in the fracture repair space.
Customizable and resorbable screws, plates and pins have evolved to improve fracture fixation and promote better bone healing, while often reducing the need for subsequent implant removal surgeries.
Biologic agents, such as bone morphogenetic proteins (BMPs), platelet-rich plasma (PRP) and stem cells enhance bone healing and promote faster repairs. Synthetic bone graft substitutes are being developed to replace or augment traditional grafts.
Additively manufactured biomaterials with enhanced mechanical properties allow for precise personalization and placement of plates and implants based on a patient’s unique anatomy.
These wide-ranging solutions have revolutionized trauma care by making fracture repair more precise and individualized, resulting in improved fixations and optimal outcomes.
Considering that approximately two million people in the U.S. experience fragility fractures each year — that number is expected to at least double by 2040 as the population ages — the need for more advanced fracture treatment technology is becoming increasingly vital.
Additionally, falls from standing height and other low-energy trauma account for 87% of all orthopedic fractures. Finding new ways to treat these injuries more efficiently and with far less recovery time is becoming an appealing and necessary advancement in orthopedic care.
Filling in the Gaps
RevBio is at the forefront of new options in fracture fixation. The company’s researchers have created a regenerative bone adhesive called Tetranite for repairing vertebral compression and extremity fractures. The material is administered through minimally invasive percutaneous injections and hardens within minutes to fixate bone fragments and provide load-bearing strength.
Tetranite is also being used to augment metal hardware fixation to fill in bone gaps and improve load sharing between the hardware and the bone itself. The adhesive allows for personalized treatment by filling the irregular gaps of missing or damaged bone, while also providing immediate fixation strength for adherence of bone fragments, according to Brian Hess, RevBio’s CEO and Founder.
“The potential benefits of personalized fracture repair are improved patient outcomes, including lower incidents of adverse effects, accelerated return to activity and better quality of life,” Hess said.
Tetranite also eliminates the need for surgeons to choose among a complex combination of hardware components to fix specific fractures, according to Hess. “Providing patients with personalized fracture repair might allow surgeons to utilize earlier weight-bearing protocols and decrease a patient’s length of stay in a hospital,” he added.
The injectable material is reacted in an aqueous-based medium to form a tacky, injectable glue that is self-setting in a wet or dry field. A contrast agent is added to the formulation, allowing surgeons to visualize the placement of the adhesive with imaging during percutaneous injection or on postoperative radiographs. The formulation can also be tuned to form a more porous structure with a specific surface area to facilitate faster resorption and bony ingrowth.
“These benefits are designed to improve patient healing and reduce the risk of malunion and nonunion in treated fractures, which leads to a lower number of revision surgeries across various patient populations,” Hess said.
Tetranite is resorbed and replaced by new bone over time, and its formulation can be tuned to match the patient’s bone density, which is especially important in vertebral augmentations.
“Patients with vertebral compression fractures typically suffer from osteopenia or osteoporosis,” Hess explained. “The mismatch in stiffness between the surrounding bone and fractures treated with polymethylmethacrylate (PMMA) cement is a known cause of adjacent vertebral segment degeneration.”
Most fractures are still treated with external fixation, percutaneous pinning with K-wires or conventional open reduction and internal fixation involving the use of locking plates. However, Hess believes the transition to less invasive solutions will ramp up when surgeons consider the risks associated with traditional techniques.
Nonunion and malunion repairs and hardware failure remain significant causes of revision surgery. Hess said fracture repair complication rates as high as 36% have been reported and can lead to the onset of complex regional pain syndrome, tendon irritation and rupture and deep infection. These complications can lead to difficulty performing basic daily tasks, loss of independence, reduction in quality of life and increased mortality.
According to Hess, early testing and human clinical trials show that new fracture repair technology poses far less risk to patients while greatly improving the current standard of care. He predicts solutions like Tetranite will become more commercially viable to provide surgeons with proven personalized treatment strategies that accelerate healing, mitigate complications and reduce the need for revisions.
“This technology can transform bone repair,” Hess said. “It has the potential to treat comminuted open and nonunion fractures, and augment the use of plates and screws, the fixation of intramedullary osseointegrated implants and the use of porous metals that rely on bony ingrowth for fixation.”
Future industry efforts will optimize personalized solutions for the treatment of high-energy extremity fractures, providing patients with a more rapid return to normal life activities, according to Hess. “This technology can eventually be assessed to treat other challenges in the field of reconstructive orthopedic surgery, including prosthetic joint stabilization, segmental bone loss and deformity correction,” he said.
Focusing on the Pelvis
Steve Dimmer, CEO of CurvaFix, has spent the past 30 years working in medical technology. Most recently he’s led the company’s development of fracture treatments specifically designed for the pelvis.
“Pelvic fractures that are left unfixed can cause considerable pain for patients, leading to immobility and other significant health issues,” Dimmer said.
The CurvaFix IM Implant is the first intramedullary implantable device that can follow the natural curved bone of the pelvis and fill in gaps caused by trauma. Unlike straight screws that don’t curve within intramedullary pathways or invasive bone plates, CurvaFix IM provides a new treatment option that’s less invasive. The device is designed to reduce pain and increase the potential for early mobility in hip fracture patients.
Dimmer said that existing technologies don’t always work very well for geriatric patients with fragility fractures of the pelvis (FFP), a problem that is estimated to affect 150,000 adults in the U.S., 80% of whom are women who are likely also suffering from osteoporosis.
According to Dimmer, a large body of clinical evidence suggests that surgery should be considered for most geriatric FFP patients, yet only 10% undergo surgical treatments because of age-related risks and other health challenges. “Non-operative, conservative treatments often lead to a worsening of symptoms, lengthy hospitalizations, nursing home admittance and high mortality rates among this high-risk patient population,” he said.
In contrast, decades of innovation in hip fracture repair have shown that strong, stable surgical fracture fixation works. Geriatric patients who undergo hip fracture repair surgery experience reduced pain and are often able to mobilize soon after procedures are completed. CurvaFix IM can improve these outcomes further, according to Dimmer.
The implant is designed to simplify surgery and provide strong, stable and curved fixation. “Surgeons report that this novel device offers geriatric patients an immediate reduction in pain and early mobility, both critically important factors for positive outcomes,” Dimmer said.
A primary advantage of CurvaFix IM is that it allows the loads supported by the pelvis during daily activities and ambulation to be distributed across the pelvic bones and the longer, wider and curved implant. This load distribution increases the likelihood that patients will be able to mobilize while their fracture is healing, which can take up to 12 weeks.
Published literature suggests that approximately 80% of FFP patients would benefit from fracture repair surgery verses conservative management, potentially increasing the number of FFP fracture repairs from 15,000 to 108,000 in the U.S. each year.
Today’s surgical fixation modalities have inherent limitations and challenges for older patients, according to Dimmer. He noted the incompatibility of straight screws in extremely curved anatomy, delayed mobilization, implant failure necessitating additional procedures, large incisions leading to high blood loss and longer surgical times and a higher risk of infection.
“Patients with curved boney pathways, anatomical abnormalities or existing hardware benefit from a curved fracture fixation device,” Dimmer said. “It can be steered through very curved or abnormal anatomy and around existing hardware.”
To date, more than 250 patients, 60% of whom are geriatric or have FFP, have been treated with CurvaFix IM. Dimmer said the device has a very low revision rate of approximately 1%, which is much lower than standard hip fracture fixation devices. Surgeons also indicate that the curved design makes implant placement safer and patient outcomes more predictable and favorable in terms of reductions in postoperative pain.
Addressing Unmet Clinical Needs
A study conducted at Michigan Medicine and published in JAMA Network Open suggests that personalized treatments of fractures are the best approach.
“Traditionally, surgeons look at broken bones on x-rays and assess the pros and cons of various ways to fix them based on feature anatomy and the patient’s age,” said Kevin Chung, M.D., a professor of surgery at Michigan Medicine and lead author of the study. “However, we determined that patient-centered care involves tailoring treatments to the specific clinical needs of individual patients and that their social environments and risk tolerance for surgery should be included in the considerations of prescribing treatment.”
Dimmer said that alternative treatments that are less invasive could be a determining factor in molding the best type of personalized care. He ultimately wants to see CurvaFix play an important role in spotlighting the unmet clinical needs of fracture repair patients by providing the necessary tools and education needed to cause a paradigm shift in their treatment.
“We are working closely with key opinion leaders within the orthopedic trauma segment to launch an initiative focused on the education of healthcare professionals within the patient care pathway,” Dimmer said. “We are also helping to educate patients and their families and connect them with specialists in their communities.”
It’s a proactive and personalized approach to fracture repair that is becoming more of a focus among surgeons and device manufacturers that will ultimately benefit patients who could use a break from traditional techniques.
NHM
Natalie Hope McDonald is a contributing editor.




