Sponsored
Healthcare is a rapidly transforming field. Changes abound—less-invasive surgical procedures, smaller and more complex orthopedic devices, disposable instruments, increased regulation, new sterilization methods, point-of-care treatments and strong emphasis on improved patient outcomes and reduced costs.
In response, Industry 4.0 technologies have come to medical device manufacturing, including Internet of Things, automation and especially additive manufacturing (AM)/3D printing. AM improves operational efficiency (in-house tools and fixtures, prototypes of parts and devices), enhances traditional machining methods or can make complete medical devices. In addition, AM materials, machines and methods have advanced to the point where commercial mass-production of medical devices is a reality.
Forward-thinking medical device manufacturers have embraced the benefits of AM in designing their devices, implants and instruments. In fact, medical engineers are designing one-of-a-kind products that can only be manufactured with AM. A growing number of device manufacturers rely on AM materials, hardware, software and services to design end-to-end workflows that reduce the number of processing steps and components for a device, thereby reducing overall cost of manufacturing, shortening lead times and speeding time to market.
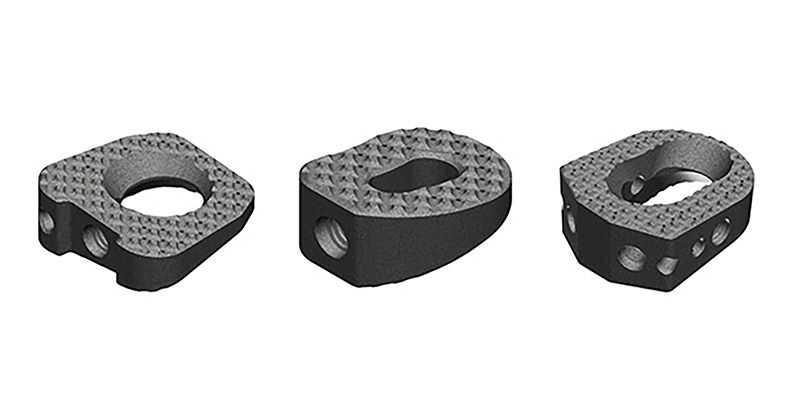
The most mature AM segment in orthopedics is the spine industry, where in the past, interbody fusion devices were almost exclusively made using traditional subtractive manufacturing processes. Now the spine industry has adopted 3D printing to introduce new revolutionary devices that can improve osseointegration, such as implants with porous or textured surfaces.1
Integrating AM into Medical Device Manufacturing Workflow
Medical device manufacturing is one of the most highly regulated processes—as such, when you choose to integrate this game-changing technology into your own business, there are several considerations to ensure success.
The first, and most significant, regards the qualification and validation of your solution. This extends beyond your materials and hardware into your supply chain. Qualifying new materials for 3D printing technology in healthcare presents challenges at multiple levels. For example, the material must be qualified for its biocompatibility and ability to meet mechanical requirements for multiple applications. The regulatory and financial burden of such qualification and the associated time can be substantial. Whenever possible, it is faster, easier and less expensive to qualify already-proven materials like 17-4 PH stainless steel and validate them for new printing applications.
The second challenge regards machine hardware engineering. Validating and optimizing parameters to run new materials can be challenging and too costly to undertake, unless there is a compelling business case for a clinical application that requires large-scale manufacturing.
Third, securing a logistics ecosystem for reliable sourcing of materials and equipment can also be a challenging task. Bringing in an experienced AM contract manufacturer to assist with product design, material selection, manufacturing and even the ever-changing regulatory landscape streamlines the entire process, avoids pitfalls and gets innovative devices to market faster, at lower cost.
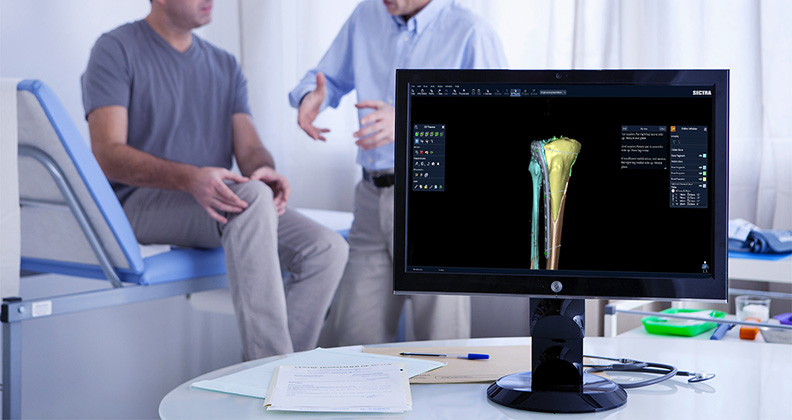
Beyond Device Manufacturing: The Future of AM
Continuing advances in AM technologies make it possible to 3D print complex medical devices and instruments from a variety of materials, including polymers, ceramics and metals, faster and at less cost than traditional subtractive machining methods. AM also plays a key role in virtual surgical planning (VSP), a service-based approach to personalized surgery that combines expertise in medical imaging, surgical simulation and 3D printing. Following an online planning session between biomedical engineers and the surgeon, patient-specific models, personalized surgical tools and instruments are designed and 3D-printed for use within the sterile field. This provides surgeons with a clear 3D visualization of a patient’s anatomy and the opportunity to develop and practice a customized surgical plan prior to entering the operating room. VSP improves surgical accuracy and outcomes, benefitting both surgeon and patient.2,3,4
M&A Requires a Harmonized Approach
Consolidations continue to occur in the spine and orthopedic industries. Small and medium-sized companies with innovative product portfolios are being acquired by large medical device manufacturers to leverage expertise and geographic reach to expand their footprint. While these companies are expanding, new contract manufacturers continue to enter the market to help address these capacity demands in an outsourced fashion. Manufacturers and service bureaus, however, utilize a variety of additive technology platforms in different ways, which can create a complex and sometimes inefficient ecosystem of novice and experienced players using multiple technologies to make a variety of implants and instruments. To counter this, the industry would benefit from a harmonized validation approach that requires devices to meet the highest quality standards demanded by the healthcare industry. For example, robust process validations and build qualifications through witness coupons would result in elevated confidence that chemically and mechanically conforming parts are produced consistently.
AM provides orthopedic device manufacturers with design freedom and operational efficiency. As more device manufacturers and contract manufacturers realize these benefits, harmonization of validated approaches will be needed to ensure the continuation of AM innovation in orthopedics.
References
1. Gupta, G: OsseoTi porous metal for enhanced bone integration – an animal study. Study completed August 2012.
2. Sink J, Hamlar D, Kademani D, Khariwala SS: Computer-aided stereolithography for presurgical planning in fibula free tissue reconstruction of the mandible. J Reconstr Microsurg 28:395-404, 2012
3. Patel A, Levine J, Brecht L, Saadeh P, Hirsch DL: Digital technologies in mandibular pathology and reconstruction. Atlas Oral Maxillofacial Surg Clin N Am 20:95-106, 2012
4. Roser SM, Ramachandra S, Blair H, Grist W, Carlson GW, Christensen AM, Weimer KA, Steed MB: The accuracy of virtual surgical planning in free fibula mandibular reconstruction: comparison of planned and final results. J Oral Maxillofac Surg 68:2824-2832, 2010
Gautam Gupta is Vice President, Global Go to Market, Healthcare, 3D Systems.