
Orthopedic product development engineers that want to tap into the potential of additive manufacturing (AM) to create groundbreaking devices often focus on designing intricate lattice geometries and constructs that improve structural support. They use AM to quickly prototype, test and refine designs, accelerating innovation and reducing time to market.
That’s a good place to start. But several experts believe it’s the materials that matter most in determining what’s possible in expanding AM’s use to produce implants that have the potential to outperform devices made with traditional metals. Here are three materials that are garnering a great deal of attention among product development teams.
Bioceramics
AM is on a fast growth trajectory, according to Craig Rosenblum, President of Himed, who said recent projections show the ceramics segment evolving into a $1 billion market by 2032. Within that potential, he added, bioactive and bioresorbable ceramics represent a significant and largely untapped opportunity in orthopedic applications.
He called out bioactive hydroxyapatite (HA) and bioresorbable tricalcium phosphate (TCP), two materials with distinct profiles and applications in orthopedics and bone repair. HA promotes a strong osteogenic response and is very stable compared to bioresorbable ceramics. TCP typically resorbs within a matter of months, compared to HA coatings that may take significantly longer, and is used in applications where eventual replacement by natural bone is desired.
Himed employs a CeraFab S65 ceramic printer developed by Lithoz. The bio ink comprises HA or TCP powder mixed with a polymer to form a printable slurry, which is dispensed into a transparent vat. Beneath the vat is a sophisticated optical system that projects blue light through the slurry.
Using a CAD file, the printer selectively cures the material layer by layer with high precision. The blue light hardens each cross-section of the design as the build plate moves in and out of the vat, gradually forming a full 3D structure. About 150 layers can be printed per hour, with each layer as fine as 10 microns.
Rosenblum said that during evaluations of candidates for a 3D-printed ceramic slurry or ink, the properties of the material are important. “The material needs to flow well,” he explained. “And the powder that’s used to create the slurry must have the right particle shape, size distribution, morphology and surface area. Those parameters are critical.”
He noted that the slurry needs to be viscous enough when printing ceramics to ensure proper densification, which plays a vital role in producing mechanically sound ceramic components.
“Ceramics are incredibly strong and highly heat-resistant, but they’re also brittle,” Rosenblum said. “That’s the trade-off, which is why material properties and processing control are absolutely essential.”
He also pointed out that ceramics shrink after a part is sintered. Because of this inherent shrinkage, designers must account for densification for ceramics to realize their true hardness potential.
Rosemblum believes ceramics are well suited for producing patient-specific implants and very small, complex parts. “With this technology, we can create devices with exact geometries and tailored porosity, features that conventional manufacturing just can’t deliver,” he said.
The potential of multi-material 3D printing in mitigating the brittle properties of ceramics excites Rosenblum. Himed has offered biphasic calcium phosphate — a homogeneous blend of 20% HA and tricalcium 80% TCP — but what’s especially promising is the potential to go beyond homogeneous blends with multi-material printing technology.
“Imagine being able to print two materials simultaneously,” Rosenblum said. “You could create a device where one end is rich in HA and the other is rich in TCP.”
Tantalum
Tantalum is drawing increasing interest because of its biocompatibility and potential to revolutionize the design of load-bearing implants.
“We believe it has tremendous potential,” said Bryan Naab, Ph.D., Additive Manufacturing Engineer at Croom Medical. “And we’re especially excited about what we can do with it through 3D printing.”
To highlight the tantalum’s potential, Dr. Naab ran through the inherent limitations of traditional implant metals.
Stainless steel is cost-effective, easy to machine and strong but it has lower corrosion resistance, high stiffness that can lead to stress shielding and potential nickel allergy concerns.
Cobalt chrome offers exceptional wear resistance and strength, but its high stiffness and the risk of metal ion leaching into the bloodstream can be problematic.
Titanium has fatigue strength for load-bearing applications and is biocompatible, but it’s also costly, difficult to machine and alloys carry the concern of aluminum or vanadium ion leaching, leading to localized toxicity effects.
Tantalum is gaining recognition for its outstanding biocompatibility and osseointegration, properties that are especially critical for orthopedic implants. What sets tantalum apart from traditional metals is its ability to bond directly with bone, according to Dr. Naab. It’s been shown to outperform titanium and cobalt chrome in terms of bone ingrowth, primarily due to the oxide layered forms and because it can be printed in pure form, meaning no alloying additions leach out.
“It also exhibits extremely high ductility,” Dr. Nabb said. “That’s important because it leads to a very predictable failure mode. Unlike brittle materials, tantalum fails in a much more controlled manner, making it easier to design implants around.”
One of tantalum’s standout features is its ability to form a strong bond with titanium. With AM, device designers can take advantage of the bulk mechanical properties of titanium and combine them with the surface characteristics of tantalum. When a tantalum structure is printed directly onto a titanium base and tension is applied, the failure occurs at the tantalum portion, not at the bond.
This makes tantalum a highly versatile material for orthopedic implants. “You could use it as part of a hybrid construct at the bone interface,” Dr. Naab said. “Titanium or cobalt chrome could serve as the bulk load carrying material.”
However, tantalum comes with inherent manufacturing challenges. “It’s expensive and difficult to scale with respect to subtractive manufacturing,” Dr. Naab said. “That’s where AM becomes key. If we want to unlock the unique advantages of tantalum, additive is the ideal technology to use.”
Tantalum produces lightweight, cost-effective lattice structures that serve as the bone interface portion of an implant. The structures can be printed directly onto titanium or cobalt chrome.
To optimize this capability, Croom Medical has partnered with Global Advanced Metals, a supplier of high-quality, ethically sourced tantalum powder. The companies have launched a printing platform called TALOS, which customers can leverage to develop new and innovative implants.
The TALOS platform is built around a dedicated GE Concept Laser M2 printer configured exclusively for tantalum. With a stable powder supply and a tightly controlled print environment, Croom can support everything from rapid prototyping to full-scale serial production.
“We’ve optimized process parameters for printing bulk, lattice structures and tantalum/titanium interface printing in really high densities,” Dr. Naab said.
He explained that Croom is currently working within the constraints of laser powder bed fusion printing to explore dual-material printing. “It’s a layer-by-layer process, so we can really only print onto flat surfaces with that particular technology,” he said.
While there are other AM techniques that could overcome this limitation, such as fused deposition modeling with multi-axis systems capable of printing onto curved surfaces, Dr. Naab noted that those options are not yet part of Croom’s current workflow.
For now, the company is focused on maximizing the potential of powder bed fusion by developing a hybrid approach that combines additive and subtractive manufacturing methods. “The way we can still make use of this dual-material concept is to print lattice onto a flat surface of titanium and then machine that part to achieve whatever geometry we want,” Dr. Naab said.
Croom’s AM setup uses a custom approach to keep costs manageable. “We have a build plate made of titanium in which we insert small titanium inserts,” Dr. Naab said. “We can print directly onto those inserts, remove them quickly and avoid the high cost of printing directly onto the entire plate.”
This modular method allows Croom’s team to perform experimental tests efficiently, enabling rapid iteration and prototyping of parts with lattice structures on top and complex geometries. It’s been a practical solution for investigating dual-material applications using laser powder bed fusion.
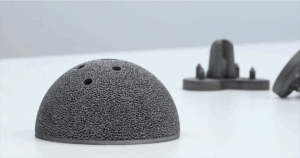
Acetabular cup implants 3D-printed in tantalum by Croom Medical.
Resorbable Polymers
Poly-Med focuses on expanding the AM applications of resorbable materials and custom polymer synthesis. To increase the regenerative potential of their printed parts, the company has also developed composite formulations that incorporate bioactive ceramics such as β-tricalcium phosphate (β-TCP) and bioactive glass.
“We’ve worked on high-tolerance parts that are fully porous and custom-fit based on CT data,” said Scott Taylor, Ph.D., Chief Technology Officer at Poly-Med. “With these composite materials, we’re seeing strong bony integration throughout the lattice structures.”
Thermoplastics have been around for decades, dating back to the 1970s with the introduction of absorbable sutures, Dr. Taylor explained. But, he added, to fully leverage the benefits of high-resolution 3D printing, especially in medical applications, a need arose to develop a new class of materials: light-curable polymers that are not only biocompatible from the outset but remain that way throughout their degradation timeline.
These next-generation polymers must be engineered to produce byproducts as they degrade, and they need to offer a range of mechanical properties that can be printed with high accuracy using various 3D printing techniques. “We’ve done a lot of work with Formlabs,” Dr. Taylor said, “but what’s exciting is that these materials are process-agnostic. They can be printed on a number of different printers.”
The flexibility of polymers has opened the door to a variety of structural designs. Poly-Med has explored foam structures, traditional cellular scaffolds and Voronoi patterns. Depending on the mechanical requirements of the final part, one infill strategy may be more appropriate than another.
Some of Poly-Med’s work involves developing platforms that support the differentiation of cells into various forms of cartilage. As the cells mature, the material gradually degrades, ultimately leaving behind only the cellular product.
“We see tremendous potential in these materials,” Dr. Taylor said. “They provide an initial performance characteristic that gradually disappears over time. Ideally, you’re left with high-quality healing and no residual foreign material challenges associated with more traditional plastics.”
Poly-Med’s approach centers on tailoring absorbable devices to meet specific clinical needs. “We don’t hold ourselves to any rigid idea of what a device should be until we understand the actual ‘why’ of the need for a bioabsorbable implant,” Dr. Taylor said.
DC
Dan Cook is a Senior Editor at ORTHOWORLD. He develops content focused on important industry trends, top thought leaders and innovative technologies.




