A new study published in Advanced Engineering Materials Journal shows how cells are sensitive to topology and thus can be exploited to help tissue heal faster. The research further validates the use of additive manufacturing or 3D printing in orthopedic implant design.
The study, led by Carmen Torres-Sanchez, Ph.D., a Reader in Multifunctional Materials Manufacturing at Loughborough University, tested implant designs currently in use and compared them to novel designs to better understand the structures bone-building cells favor. Dr. Torres-Sanchez and her team were able to accelerate bone healing by tweaking implant designs.
An important part of the orthopedic research was to examine the biological and mechanical performance of design topology simultaneously. Dr. Torres-Sanchez noted that research is often siloed, looking at either the mechanical properties of porous scaffolds or the bioengineering side of how cells change and mature.
“It is seldom the case that both aspects of the scaffolds’ performance are considered at the same time. What could be the best scaffold design in terms of mechanical properties may not be favored by the osteoblasts, and vice-versa,” she said. “But we knew we needed to work with both aspects concurrently, always keeping at the forefront of our mind what the end goal is: to optimize the scaffold for implantation. This involves interrogating the scaffold on both the physical-mechanical properties and its bioengineering behavior.”
Implant Designs
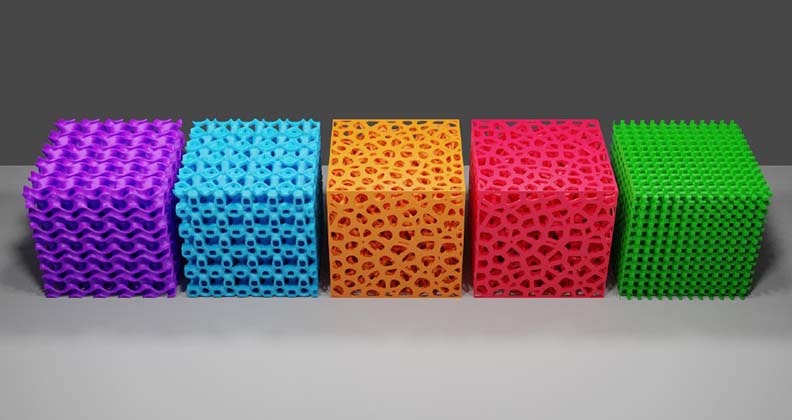
The research involved testing triply periodic minimal surfaces (TPMS) and trabecular-like structures by 3D printing, specifically selective laser melting, cubes or scaffolds out of titanium.
The mechanical properties of the scaffolds were tested by applying forces that replicate the physiological loads that orthopedic implants would be subjected to in the body. The goal was to determine whether the new designs could withstand loads and at which point they would fail. The biological performance of the designs was assessed by adding precursor cells to osteoblasts (bone-building cells) to the inside of the scaffolds. The aim was to see if the cells evolved into mineral matter, which forms bone.
Ultimately, the researchers found that cells prefer the more random distribution of porosity, such as that seen in trabecular scaffolds.
TPMS is currently very fashionable, Dr. Torres-Sanchez said. Derived from mathematical equations, TPMS is repetitive unit cells connected to form a pattern of interconnected pores. Using Voronoi partitioning for the trabecular-like structures, the researchers created randomly distributed trusses and beams that resemble the actual geometry of the trabecular bone.
“We compared those two types of topologies to a control, this is, a typical regular lattice structure used in implants,” Dr. Torres-Sanches said. “We validated the scaffolds from physical, mechanical and also biological viewpoints and concluded that osteogenesis, not only prefer topologies that mimic natural structures (the trabecular-like structures) but also have a predilection for rounded pores and cavities, with a surface roughness that is inviting for the filopodia (these are the anchors of the cells that attach to the substrate), because the dimensions of the peaks-and-troughs of that jagged surface match their size. Like a good fitting of a shoe to a foot.”
She added that the study findings show that engineers can contribute to getting patients back to their everyday life sooner by providing designs and scaffolds that promote healing and help speed up patient recovery.
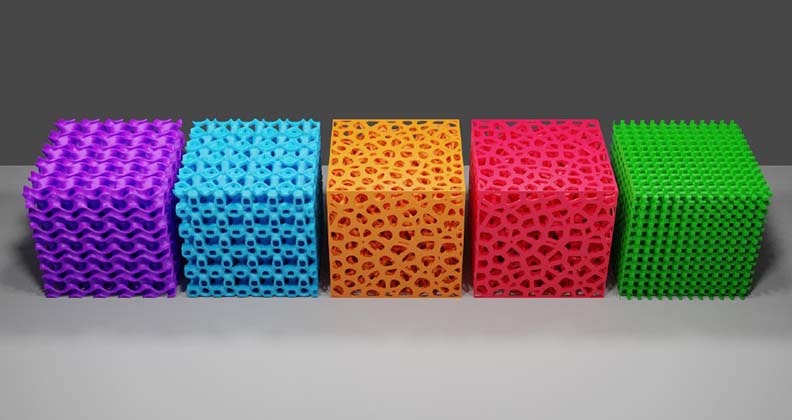
Different scaffold designs were used in the study (CAD image). From left to right: two TPMS-type structures, two trabecular-like structures, and a lattice structure, which was used as a control scaffold.
Research in Action
Dr. Torres-Sanchez said she hopes her research will assist in future clinical applications for trauma and bone cancer patients, who could benefit from implant designs that promote bone growth. But she noted that additive manufacturing in orthopedics offers great flexibility at the design stage and unconstrained manufacturing. Its use, along with her study findings, can be applied across orthopedics.
“There is much effort from both clinicians and orthopedic manufacturers put into the design of tailored, personalized implants with the trials of different topologies and shapes. We have demonstrated through this systematic comparison which topologies are preferred by the bone-building cells and which are not. We hope this will help speed up the translation of efficient microarchitectures into products that can be implanted successfully and long term by focusing on the structures that have potential and discarding those that don’t,” she said.
“We have also shown that it is possible to improve the cell-scaffold interaction by tweaking the design, making it even more favorable, e.g., rounding off the edges and preventing sharp corners. This opens a door to the personalization of scaffolds to the patient, and within the same patient, tailoring it to the actual anatomical location that requires the implant.”
Next Study Steps
With the publishing of her recent study findings, Dr. Torres-Sanchez and her team look to advance their research. The researchers will continue finetuning implant designs so that they can find subsequent evolutions of multifunctional scaffolds that are even more appealing to the body’s cells.
The research includes working on new alloys that can be bioinstructive. The goal is to identify how the physical microarchitecture helps the healing process and how the chemistry aids the rightly paced recovery of compromised bone.
“We are looking into materials that support the cells in their maturation journey,” Dr. Torres-Sanchez said. “Once the host tissue has regenerated and consolidated, the scaffold can disappear, be eaten up by the body and digested, so the patient does not feel its presence, for example, when the weather changes.”
CL
Carolyn LaWell is ORTHOWORLD's Chief Content Officer. She joined ORTHOWORLD in 2012 to oversee its editorial and industry education. She previously served in editor roles at B2B magazines and newspapers.




