Researchers at the National University of Singapore (NUS) have discovered that stem cells can be cued to turn into bone when they’re squeezed through tight spaces.
Instead of using growth factors or genetic manipulation, the researchers found that mechanically compressing cells during migration activates bone-specific genes. The work adds to a growing understanding that physical forces play a critical role in shaping the way cells develop and function — and could change how regenerative therapies are designed.
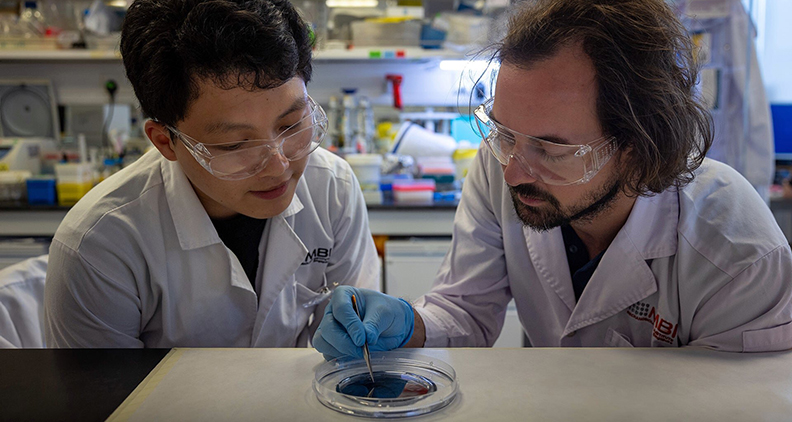
Andrew W. Holle, Ph.D., led the research, which was published in the journal Advanced Science.
“I’ve been studying cellular responses to physiological confinement since my postdoc work,” said Dr. Holle, Assistant Professor in the Department of Biomedical Engineering at NUS and Principal Investigator at the Mechanobiology Institute in Singapore. “I became fascinated with the idea that other types of cells, beyond cancer and immune cells, could be influenced by mechanical confinement. This project was a combination of that experience and my Ph.D. work with stem cells.”
Memorable Squeeze
Dr. Holle’s team focused on mesenchymal stem cells (MSCs), which are adult stem cells found in bone marrow and other tissues. The cells can develop into bone, cartilage or fat, making them a key tool for regenerative medicine.
To test how physical forces influence stem cells, Dr. Holle’s team developed a specialized microchannel system that mimics the narrow tissue spaces that cells navigate in the body. When MSCs were forced to squeeze through the narrow channels, they began to express RUNX2, a gene linked to early bone formation.
The effect persisted long after the cells had passed through the channels, suggesting they retained a mechanical “memory.”
“We’re still working to understand this memory,” Dr. Holle said. “But our data show that simple nuclear deformation at the right magnitude and duration could provide the stimulus needed to initiate differentiation. Even without pulling from the cytoskeleton, compression alone can push cells toward an osteogenic lineage.”
Dr. Holle’s team noticed that other lineage-specific genes that are tied to fat and cartilage also increased after confinement, but only the bone-related factors moved into the nucleus, where they can influence what cells turn into.
“We were surprised that this confining journey seemed to cause the overall levels of a number of lineage-specific transcription factors to increase, including fat and cartilage,” Dr. Holle said. “However, only the osteogenic ones exhibited an increase in nuclear translocation, which is the most important event for regulating cell fate.
“The balance between differential transcription and differential translocation seems to be really important, and we definitely want to dive deeper into that in the future.”
Scaling Up
The idea that compression can prompt long-term changes in cell behavior challenges older models that focus mostly on chemical signaling. It also offers a more scalable approach for directing stem cells’ fate in a lab or clinical setting.
Traditional stem cell conditioning methods rely on soluble factors, which can be costly and difficult to reproduce consistently. Physical confinement could offer a simpler, cheaper and safer alternative or complement to existing practices.
“We don’t think biochemical approaches will go away, but we do believe that most future protocols will include some physical component,” Dr. Holle said. “Confinement is a great place to start. The method requires no chemicals or genetic modification — just a maze for the cells to crawl through. In theory, you could scale it up to collect millions of preconditioned cells for therapeutic use.”
Applying confinement practices in an effective way will require new tools. The current setup works for small batches of cells. Scaling it up for clinical use will mean developing devices that can handle millions of cells.
“The tools we have now can yield hundreds of cells, enough for imaging or small-scale experiments,” Dr. Holle said. “For therapy, we need orders of magnitude more. We’re working on some clever solutions to make that possible.”
Building Bone
Cells that have been mechanically primed to become bone could be introduced into injury sites or defects to speed healing or improve outcomes in challenging cases.
“It’s easy to imagine a workflow where you take patient cells, expand and mechanically precondition them, and then reinject them,” Dr. Holle said. “That kind of setup could reduce reliance on synthetic implants or donor grafts.”
His team is also planning to use animal studies to test if post-confinement cells can complete the full process of bone formation, not just initiate it.
“We’d love to test these cells in models of bone injury to see if they really improve healing,” Dr. Holle said. “That’s the next step.”
New Guidance
Dr. Holle’s work adds to the growing field of mechanobiology, which examines how cells sense and respond to physical forces. While chemical signals have long dominated biomedical research, there’s a shift toward understanding how mechanical stress influences cell fate.
His lab puts confinement at the center of this movement. As more researchers adopt mechanical conditioning tools, the hope is to create faster, cheaper and more reproducible ways to produce therapeutic cells that are tuned not just chemically, but physically, to improve their healing properties.
The approach could one day be used to speed recovery from bone fractures or enhance the effectiveness of stem cell therapies.
“Most people think of stem cell fate as being determined by chemical signals,” Dr. Holle said. “What our work shows is that physical confinement alone can also be a powerful trigger for differentiation.”
DC
Dan Cook is a Senior Editor at ORTHOWORLD. He develops content focused on important industry trends, top thought leaders and innovative technologies.




