Orthopedic surgery is undergoing a revolution in which smaller truly means better. A new wave of minimally invasive implants and instruments is reshaping the ways surgeons treat patients. These cutting-edge designs promise faster recoveries, reduced scarring and improved patient satisfaction — all while overcoming the engineering challenges of strength, durability and precision.
The transformation of minimally invasive solutions proves that smaller implants can achieve remarkable results and expand the possibilities of modern orthopedic care. “Today’s patients demand procedures that get them back to work and life faster,” said Travis Greenhalgh, CEO of SurGenTec. “If companies don’t develop these types of devices and surgeons don’t adopt them, they risk being left behind.”
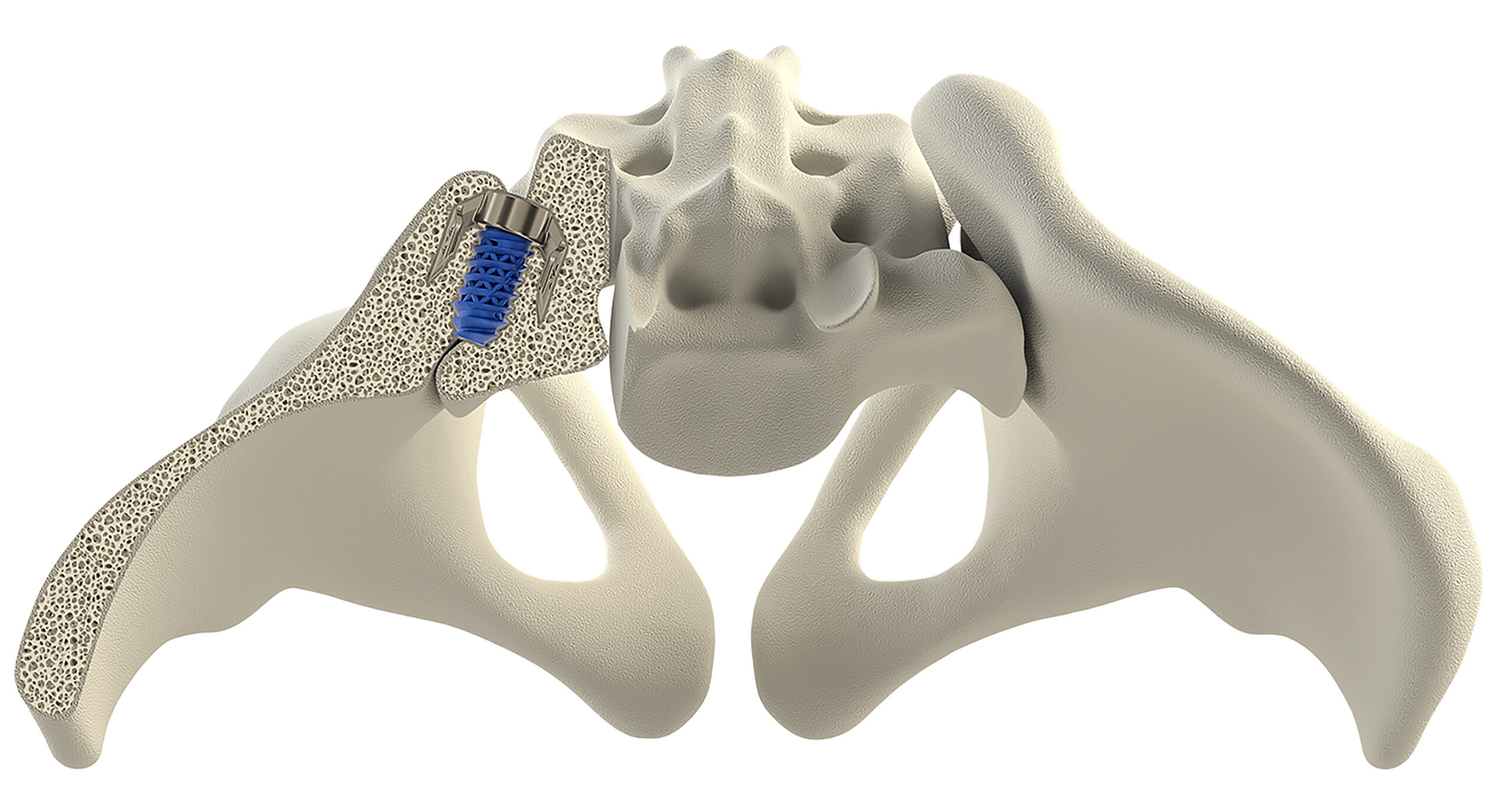
SurGenTec is exploring novel ways to reduce patients’ pain while minimizing incision and implant sizes. One of its most notable advancements is the TiLink-P implant for sacroiliac (SI) joint pain. “TiLink-P combines the principles of compression and posterior implantation to stabilize the painful region with just one small incision,” Greenhalgh said.
The device is engineered to address the unique biomechanical challenges of the SI joint and resist forces such as shear, compression nutation and distraction. It integrates 3D-printed features that enhance bone graft placement and support faster, stronger fusion.
SurGenTec also developed the ION facet screw system, which uses micro implants to address painful regions of the spine. These implants are smaller than a dime — 30mm to 40mm shorter than traditional pedicle screws — to offer a less invasive option.
“ION has been used in cervical and lumbar cases, and we’ve seen that it can decrease operative times and risk of neurologic injury,” Greenhalgh said. “In general, larger implants are inherently less muscle sparing and have increased risk of nerve or vascular injury. The approach we’re using attempts to mitigate those risks.”
SurGenTec’s compact, innovative designs are particularly well-suited for ambulatory surgery centers, where efficiency and space constraints are critical.
“The minimally invasive approach to stabilizing the SI joint offers clear advantages,” Greenhalgh said. “By reducing the number of implants and the size of incisions, it simplifies procedures and decreases operative times.”
Focusing on Joint Preservation
Patients wanting less invasive procedures and faster recoveries have driven the development of smaller implants and instruments, according to Jeffrey Halbrecht, M.D., Founder, Chairman and Chief Medical Officer of ZKR Orthopedics. “It’s about creating solutions that allow surgeries to be performed through smaller incisions without compromising outcomes,” he said.
Dr. Halbrecht also highlights the shift from hospital-based surgeries to outpatient surgery centers, the growing need for cost-effective care and the rising focus on joint preservation as drivers of the minimally invasive movement. “Preserving natural anatomy is becoming a priority, as younger patients are increasingly seeking ways to manage joint issues without resorting to full replacements,” he said.
At ZKR Orthopedics, this philosophy has guided the creation of a novel approach to treating patella arthritis and led to the development of the Patella LIFT implant. The device is implanted in the knee through a 1.5-inch incision; the surgery requires no bone cutting, allows for immediate weight-bearing and eliminates the need for braces or extended post-op rehabilitation.
Patella LIFT serves as an “offloading” device, reducing pressure on the joint to alleviate pain and eliminating the need for a full knee replacement. The implant is particularly beneficial for patients who feel they are too young to have their knee replaced or those with specific cartilage conditions like chondromalacia.
“The implant not only alleviates pressure on the joint but also optimizes the biomechanical forces acting on the patella,” Dr. Halbrecht said. “By preventing excessive shear and rotational forces, it helps to maintain joint alignment while supporting faster healing. This precision is critical for achieving long-term success.”
The procedure’s benefits are significant. “Patients can walk right away and regain full range of motion in the joint almost immediately,” Dr. Halbrecht explained. “It’s a much faster recovery compared to a standard knee replacement.”
In February 2024, ZKR Orthopedics received Investigational Device Exemption (IDE) approval from FDA for a multicenter prospective PELICAN trial using the Patella LIFT implant. As part of its PELICAN IDE application, ZKR Orthopedics reported data from its first in-human trial, which reported a 62% reduction in overall patient-reported pain and a 28% improvement in patient-reported knee function. No patients progressed to partial or total knee replacement and the implant did not cause patellar tendon necrosis or tendon structural damage.
Patella LIFT’s PELICAN trial enrolled approximately 245 patients at 24 sites in the U.S. and Europe. It will evaluate patients with later stage cartilage degeneration and osteoarthritis of the patellofemoral joint. The researchers will compare the results of Patella LIFT procedures performed in the United States to a control group consisting of tibial tubercle osteotomy patients undergoing procedures in Europe. The trial’s primary endpoints consist of patient-reported outcomes, safety measures and radiographic confirmation. Joint pain and function and speed of recovery are the secondary endpoints.
The first U.S. Patella LIFT procedure was performed as part of the PELICAN trial last September at Oregon Health & Science University. The outpatient surgery lasted less than 45 minutes and allowed the patient to walk the same day.

The Patella LIFT implant from ZKR Orthopedics offers a minimally invasive alternative to knee replacement surgery.
Navigating Challenges
The development of smaller implants and instruments comes with unique obstacles, particularly in maintaining durability and ensuring precise outcomes. While minimally invasive solutions offer significant benefits, they require thoughtful design, advanced technology and rigorous testing.
One major factor driving these innovations is the adoption of 3D printing technology, which allows for creative designs that are difficult or impossible to produce with traditional manufacturing methods. However, it does have its limitations.
“While 3D printing allows for more intricate designs, it lacks the inherent strength of machined metal,” Greenhalgh said. “That’s why extensive biomechanical testing and finite element analysis are critical to ensure implants meet safety and durability standards.”
Dr. Halbrecht emphasized the importance of precise designs when creating instruments for smaller incisions. He highlighted the need for tools that allow surgeons to operate effectively in constrained spaces while maintaining fixation and alignment.
ZKR Orthopedics has prioritized precision and reliability in the development of its Patella LIFT implant. The company followed a rigorous testing protocol, starting with biomechanical and computer simulations. “The goal is always to ensure durability and effectiveness without compromising on precise and accurate placement,” Dr. Halbrecht said.
While minimally invasive innovations are promising, getting surgeons to adopt new surgical approaches and devices takes time and effort.
That reality is starting to shift the focus of surgeon education within industry and teaching institutions, which are adapting to the move toward less invasive surgical approaches by equipping new surgeons with the skills they need to meet the growing demand.
“Fellowship programs are teaching minimally invasive techniques more widely, ensuring surgeons can compete with peers already trained in the newer methods,” Greenhalgh said. “This evolution is crucial as more procedures move to ASCs, where patients need to recover faster and in less pain.”
Looking Ahead
As ZKR Orthopedics focuses on perfecting its Patella LIFT implant and procedure, it’s exploring the possibility of expanding the offloading design concept to other joints. For now, the company is dedicated to improving outcomes for patients with patellar arthritis and offering a viable alternative to traditional knee replacement surgery.
For SurGenTec, the focus remains on creating implants like the TiLink-P and ION systems, which are transforming care for spinal instability. These solutions not only improve recovery times but also address the growing demand for precision and efficiency in surgical procedures. “Ultimately, it’s all about improving patient outcomes,” Greenhalgh said. “Patients want to return to their lives as quickly and painlessly as possible, and these innovations are helping us make that a reality.”
Patients are also more informed and proactive than ever, often arriving at preoperative consultations armed with online research and specific treatment requests. This reality has created a competitive landscape for orthopedic practices and device manufacturers.
“Patients want quicker healing times, less scarring and less pain,” Greenhalgh said. “They’re dictating the direction of their care. It’s no longer about accepting the standard approach — they want their surgeries performed with the latest technologies.”
KK
Kendal Kloiber is a contributing editor.




