The key to more effective rotator cuff repairs could lie in the sharp, backward-curved teeth of pythons. Stavros Thomopoulos, Ph.D., and researchers at Columbia University have discovered a way to capitalize on the properties of the snake’s fangs to grasp soft tissue without tearing it.
“The fundamental problem with reattaching tendon to bone is the mismatch in properties between the two materials,” said Dr. Thomopoulos, the Robert E. Carroll and Jane Chace Carroll Professor of Biomechanics in Orthopedic Surgery and Biomedical Engineering at Columbia. “Suture anchor rotator cuff repairs, the current gold standard, must transfer load from tendon to bone across a few grasping points.”
The stress concentrations at these grasping points lead to suture pulling through tendon and failure of repairs, Dr. Thomopoulos noted.
That’s a significant clinical concern, according to statistics Dr. Thomopoulos’ research team published in the journal Science Advances. They noted that rotator cuff tears are among the most common tendon injuries, affecting more than 17 million people annually in the U.S.
The likelihood of these injuries rises with age, with more than 40% of individuals over 65 experiencing a rotator cuff tear that leads to shoulder pain and decreased mobility. Surgical repair is the main approach to restoring shoulder function, with over 600,000 procedures performed each year in the U.S. at a cost of $3 billion.
Since rotator cuff tears most often occur at the tendon-to-bone insertion site, the goal of surgery is to reestablish the tendon’s attachment anatomically. However, reattaching tendon to bone continues to pose a major clinical challenge.
Surgical failure rates are notably high, especially in older patients and individuals with severe tears. While failure rates are around 20% for younger patients with smaller tears, they can climb to as high as 94% in elderly patients with large tears. The Columbia researchers noted that the most frequent cause of failure in rotator cuff repairs is the sutures tearing through the tendon at the grasping points where force is concentrated.
Their biomimetic approach to solving the problem of high failure rates follows the design of python teeth to reattach tendons to bone more securely. The device they developed not only augments the strength of the repair but can also be personalized to a patient’s anatomy.
Grasping Without Tearing
While discussing the clinical need to strengthen rotator cuff repairs, one of Dr. Thomopoulos’ trainees brought to his attention that pythons trap their prey with curved teeth. This aha moment inspired the creation of a device that can securely grasp tendon while avoiding the issues inherent in suture repairs.
The device Dr. Thomopoulos’ research team designed is in the developmental stage. The team initially set out to replicate the shape of python teeth, but their work expanded through simulations, 3D printing and ex vivo experiments on cadavers. They ended up investigating the way tooth shape influences grasping versus cutting mechanics.
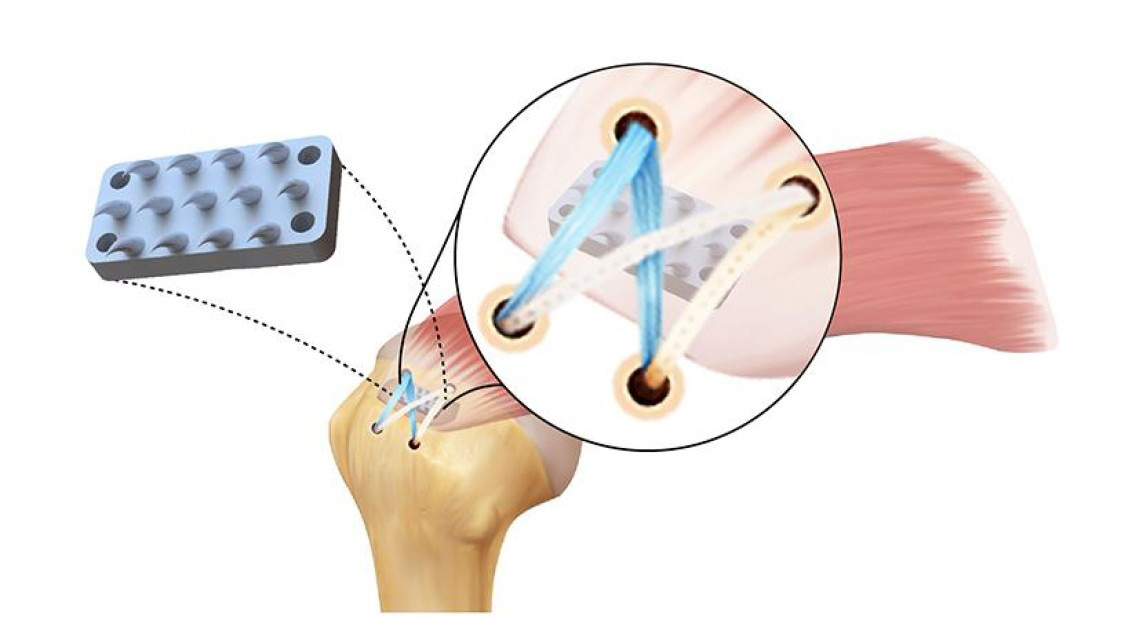
Research team member Iden Kurtaliaj, Ph.D., produced various tooth designs, optimizing individual teeth, arrays of teeth and eventually a rotator cuff-specific array. The final product was a biomimetic device made from biocompatible resin, featuring an array of teeth on a curved base designed to grasp, not cut, tissue.
These teeth, measuring about 3mm high to match a human rotator cuff — half the length of a standard staple — are small enough to avoid piercing through the tendon. The base of the device can be customized with 3D printing to match the unique curvature of the humeral head at the supraspinatus tendon attachment site, the most frequently torn tendon in rotator cuff injuries.
The researchers noted that the device is positioned strategically between the two suture anchors in the medial row to strengthen these tendon-suture interfaces, which are prone to mechanical failure. They noted that the curved teeth add significant mechanical strength to the repair due to what simulations predicted to be a more even distribution of loads across the attachment footprint.
Cadaver repairs showed that the device can double the strength of a typical rotator cuff repair. Dr. Thomopoulos said the next stage in the development of the device is to refine its design with biomaterial to make it resorbable and improve the structure by incorporating a porous base.
“For the second-generation device, we hope to incorporate biologic factors released directly from the device and seed it with autologous mesenchymal stem cells.” Dr. Thomopoulos said.
The research team tapped into the expertise of surgeons while designing the device. “Due to our laboratory’s close collaboration with orthopods, we were especially fortunate to get input from physicians at Columbia throughout the device’s development process,” he said.
Next Steps
Dr. Thomopoulos and his team established a python tooth–inspired approach for increasing repair strength immediately following rotator cuff surgery. They noted that the approach specifically addresses the leading cause of high failure rates following traditional rotator cuff repair: sutures pulling through the tendon due to tension at the medial side of the repair.
They’re very excited about the device’s potential to improve the care of rotator cuff injuries. “We expect it will substantially reduce the failure rates currently seen after rotator cuff repair,” Dr. Thomopoulos said. “Our approach suggests an alternative to traditional suturing paradigms and may reduce the risk of tendon retearing after surgery.”
The researchers are now focusing on developing a bioabsorbable version of the device, which would degrade as the rotator cuff heals back to the bone, enhancing its clinical potential. In addition, they are preparing for a pre-
DC
Dan Cook is a Senior Editor at ORTHOWORLD. He develops content focused on important industry trends, top thought leaders and innovative technologies.




